Results of Stanford’s Bionic Pancreas Study—A Patient’s Point of View
Editor’s Note: The Division of Endocrinology and Diabetes at the Stanford University Medical Center is renowned for its work in clinical research, education and care. Its clinical studies are ground breaking, helping to determine methods of better care in endocrine disorders. Under the leadership of Dr. Bruce Buckingham, clinical research is ongoing. Garrett Jensen, a graduate of Santa Clara University in accounting and political science and a person with type 1 diabetes for 10 years, is an avid promoter of clinical research and new technology that improves the lives of those living with type 1 diabetes (T1D). Currently, he works at EY in the Americas Corporate Responsibility Group and recently participated in the Stanford’s Bionic Pancreas Trial that took place over the span of three weeks in January of 2016. This is what Garrett had to say in conclusion of the study and of his involvement.
Conclusion of study
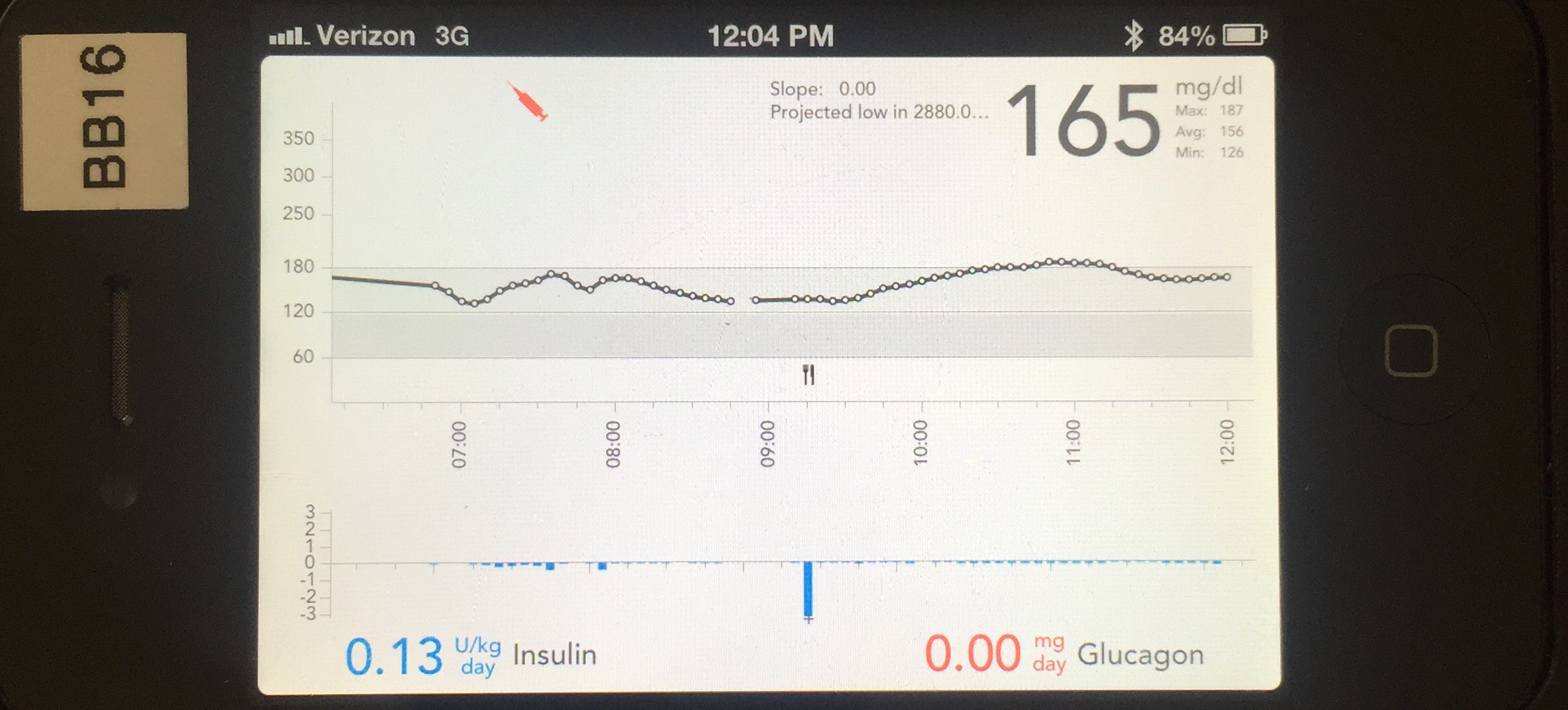
Three weeks of being on the bionic pancreas (BP) system and the results are promising. As a review, the first week was normal care, the second week was on the bionic pancreas with a set point of 7.2 mmol/L130 mg/dL, and the third week was a “dynamic set point” or blood glucose range of 6.4 to 7.2 mmol/L115 to 130 mg/dL.
From participating and listening to my fellow test subjects in a focus group, there are a number of key takeaways:
Consistency is a diabetic’s friend
We’ve known this prior to any thought of diabetes management technology. If you are consistent in schedule and diet, the system will be better at responding to your “normal” insulin needs.
If you have great control before, than this device won’t make your numbers all that much better
Don’t be discouraged by that though. It has significant impacts for you still, as well as those that need to reign in their control, young and old people, and will affect training for newly diagnosed individuals. We will all benefit from a “smart” basal mimicking the behavior of a full functioning pancreas.
It will do wonders for control freaks
On the BP, the system takes the helm and no interventions are permissible, much to the chagrin as I discovered of people with diabetes with many more years under their belt than I.
Significant reduction in “time hypoglycemic”
This is the most exciting achievement and what will really impress the FDA and insurance companies. During normal care, I was below 3.9 mmol/L70 mg/dL about 6.5 percent of the time. In using the bionic pancreas two weeks, I had a similar blood sugar average, but was low half of one percent of the time. That’s 0.5 percent. Yeah, I know, pretty amazing. What this means is that there is a far lesser risk of acute, emergency care. We know costs related to hypoglycemia have proven to burden the U.S. healthcare system substantially. Therefore, it would behoove health insurance companies to cover BP systems!
Liberated from carb counting
You must, however, still “meal declare.” You do not need to be a perfect carb counter any more. You must announce whether the meal or snack you are about to ingest is a bite, a Thanksgiving feast or somewhere in between. This allows the algorithm to learn your patterns and make judgments about insulin needs, just like Spotify does for your music.
Anyone can use it
There’s no limitation as to who can use it; its user interface is relatively simple.
What will be interesting, is to see how the bionic pancreas, now that’s it’s almost here, will adapt and how consumers will respond to the influx of companies getting into this space. Coverage is clearly the number one consideration. But will features be number two? Or maybe adaptability with other existing systems/products? And if so, what will people with diabetes go for or prefer? And what will patients be willing to pay? Some systems are planning for glucagon to be infused after additional research, while other systems may first go to a “smart” basal concept.
What is clear is that medically, technologically and economically, we are entering into a new age of diabetes management, one that will slowly alleviate the physical and psychological pressures by utilizing “smart” systems and algorithms that learn about us. The result: perhaps getting a few moments per day when we don’t consider the implications of our shared chronic disease. Lower hemoglobin A1C’s are on the horizon my friends.
On to the next study.
Read about Garrett’s perspective leading up to the study HERE.
More on Garrett Jensen





