Comparing the Dexcom G6 to the G5
As I write this, I have the highly-anticipated, recently FDA approved Dexcom G6 affixed to my belly and my Dexcom G5 on the back of my arm. I’ve had the privilege of test driving the G6 and comparing the two continuous glucose monitors from Dexcom, and I’m excited to share my findings with you!
One quick note: this is a fairly unscientific comparison of the G6 to the G5. I did not insert the two sensors at the same time and I wore them on different body parts. Like any continuous glucose monitor (CGM) user knows, each sensor is prone to issues caused by any number of variables.
Instead, this is a real-life comparison of the G5 I would have been using (and dosing off of) to the G6 over a few days. Let me take you on a G6 journey! The CGM, not the private jet.
Key differences between the G5 and G6
Before we get started, let’s review what Dexcom is promising from the new G6:
- Fingerstick elimination – No fingersticks are needed for calibration or diabetes treatment decisions.
- Easy sensor applicator – Complete redesign of the sensor applicator allows for one-touch, simple insertion.
- Discreet and low profile – A redesigned transmitter with a 28 percent lower profile than previous generation Dexcom CGMs makes the device comfortable and easy to wear under clothing.
- Acetaminophen blocking – New feature allows for more accurate blood glucose readings with no medication interference.
- Predictive low alert – New alert feature predicts hypoglycemia before it hits to help avoid dangerous low blood sugar events.
- Extended 10-day sensor – 10-day sensor allows for 43 percent longer wear than previous generation Dexcom CGMs.
G6 insertion
There were two big differences between sensor insertion for the G6 vs the G5: new auto-inserter and the addition of sensor codes.
Let’s talk a little bit about this new auto-inserter. It’s bigger, sleeker and completely hides the needle. You just press a button on the outside and the spring-loaded needle inserts the sensor and retracts super fast. It’s much more like a pump insertion than the previous G5 insertion—which for me was an improvement. I’ve been known to call the G5 insertion setup “the harpoon.” That needle is intimidating. I often need to take a deep breath and stare at an object on the ground before a sensor insertion … and I’m not particularly bothered by needles. So the hidden needle was a plus, and the quick auto-insertion definitely hurt less and was less scary than the G5 version.
One thing that surprised me was the insertion device is not reusable. Each sensor comes pre-loaded into the large white plastic device. This makes unused sensors fairly bulky, which might be annoying for packing for a long trip. It also feels like a lot of waste to throw away every time. I’ve heard it rumored that Dexcom claims it’s actually no more plastic than the G5 inserter and that there are plans to roll out a recycling program. I await more info on both! My type 1 diabetes (T1D) waste footprint is already big enough.
The other major difference I noticed upon insertion: sensor codes. With the Dexcom G5, each transmitter (the grey bit that sends a bluetooth signal to the receiver) is coded, but the sensor (the small wire that is inserted under the skin) is not. With the Dexcom G6, the transmitter AND sensor both have unique codes that must be entered into the receiver. This has to do with the FDA-approved 10 day wear time, and I imagine is designed to ensure that each sensor is only used once. Skip down to the FAQ section for more on this!
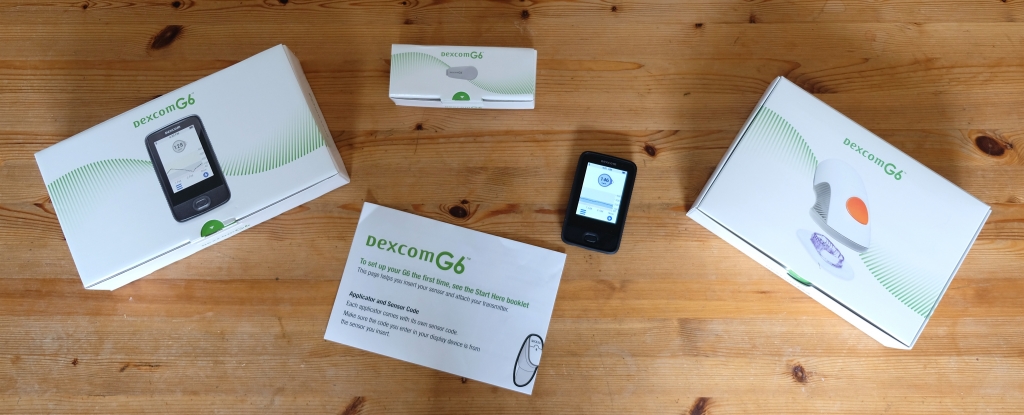
Watch the Facebook Live of unboxing and insertion!

Comparing Dexcom G5 to G6 readings
I tracked a little over 24 hours of G5 vs G6 vs fingerstick readings for comparison. But first, a quick note on accuracy: my fingerstick readings were taken with a OneTouch Verio Flex blood glucose meter, which is accurate within 15 percent for blood glucose (BG) values over 4.2 mmol/L75 mg/dL, per the device Owner’s Booklet. Put differently—95 percent of blood sugar readings taken with my meter will fall within 15 percent of the absolute value of my blood glucose. Separately, the Dexcom G5 has a 9 percent MARD rating. That’s the “mean absolute relative difference” wherein a lower rating = higher accuracy. The Dexcom G6 also has a 9 percent MARD rating, but does so without the need for fingerstick calibrations.
Basically, what I’m saying is: these numbers do not deal in absolutes. It’s impossible to know whether an actual blood glucose measurement is closest to the G5, G6, or fingerstick. But typically, we use fingerstick for calibration and reference, so that’s how I proceed here.
The first thing I do upon waking up on Friday morning is a BG check and CGM comparison.
G5: 116 / G6: 151 / Fingerstick: 142
I calibrate my G5. In my first check in, G6 is looking strong! An hour or so later, I glance back at the CGMs.
G5: 142 / G6: 146
It looks like my calibration got the G5 straightened out, and we’re cruising with a relatively flat line. Great. Before lunch, I’m back on the blood sugar beat.
G5: 144 / G6: 194 / Fingerstick: 173
Interestingly, the G5 line has remained pretty flat from earlier in the morning while the G6 is trending up. Fingerstick has me trending up too, but not up as far as the G6 does. After lunch we do another check in.
G5: 141 / G6: 183 / Fingerstick: 180
It looks to me like I did bump up a bit and my G5 never caught it, but the G6 did. I decide at this point to calibrate the G5 again. I know over-calibrations can be a problem, but I do it anyway. Later, things are more obscure.
G5: 145 / G6: 183 / Fingerstick: 162
Fingerstick is smack in the middle. I do nothing, and figure I’m somewhere between these values. Cool.
Key takeaway #1: It seemed to me like G6 caught some smaller fluctuations that G5 may not have. There could be lots of reasons why.
These numbers are all from a fairly straightforward day of in-range blood sugars without many crazy variables. I kept tracking over the weekend, when things usually get a little whackier for me. No surprise—more calories, more alcohol, and YEP, crazier blood sugars. Let’s dig in to the numbers.
Saturday morning after breakfast:
G5: 169 / G6: 229 / Fingerstick: 252
Okay, it was a pretty big breakfast. It looks to me like I’m going UP and the G6 is lagging less than the G5. Both graphs are trending similarly, but the G6 reading is closer to the fingerstick for sure. I correct with more insulin, and wait a little bit. Before lunch, we check back in.
G5: 199 / G6: 263 / Fingerstick: 264
Oof. My G5 is showing a rise in my blood sugar after breakfast (the graph went as high as 240 before coming down), but nothing compared to what I’m seeing on the G6 and in fingersticks. That’s super key because I (like many others) often use my G5 for dosing. I would have been way off here on my lunch bolus!
Let’s skip ahead to the next morning. I was blessed with a flat overnight line (thank you, BG fairies), and woke up like:
G5: 187 / G6: 171 / Fingerstick: 172
Pretty nice all around!
Key takeaway #2: It seems to me that when my blood sugar is trending relatively flat, the G5 and G6 are both close to the fingerstick numbers. When I had a high, the G6 seemed to outperform the G5 when compared to fingerstick numbers. This is only anecdotal, but hopefully a good sign!
Frequently asked questions
Is there still a 2-hour sensor warm up time?
Yes, there is. Same as the G5.
Do I need to calibrate the Dexcom G6?
No calibrations necessary, but you CAN calibrate if you feel you need to.
Can I restart the sensor after the 10-day wear time?
Unfortunately not. I have been known to stretch a G5 sensor up to three weeks if it’s working well. The G6 is FDA approved with dosing (hopefully remote via pump) in mind, so it seems like they cracked down on extended wear times to ensure accuracy for the no-calibration approval. Note: I haven’t yet tried to restart the sensor.
How much will the Dexcom G6 cost?
Cost will be dependent on your individual insurance plan. From Dexcom CEO Kevin Sayer in an interview with Beyond Type 1: “We have not negotiated pricing with all the payers; we don’t anticipate the cost of G6 to be more than G5. Certainly with label use it should not be. Part of the cost concern in the community is related to the fact that the sensor does shut off in 10 days. That was part of the FDA requirement to get the labeling that we got. If you have a sensor that you don’t calibrate and restart that algorithm will assume it’s a new sensor, which is a problem. We think it is a fair trade for patients overtime and eventually we would like to extend the life to 10-14 days.”
When will the G6 be available for everyone?
The Dexcom website FAQ says G6 will start shipping out in June! New customers will be able to get a G6 immediately. Current customers will be automatically upgraded when their G5 device goes out of warranty.
Is the G6 available outside the USA?
Not yet, but Dexcom CEO Kevin Sayer reports: “The Dexcom team has developed a detailed rollout plan to a number of OUS geographies, including Canada. We will elaborate on these plans as we obtain the appropriate international regulatory clearances for G6.”
Test drive takeaways
Overall, I would sum up my experience so far with the Dexcom G6 like this: it seems to be working the way a G5 works when it’s functioning on point. It has done so without calibrations and without interruptions. When my Dexcom G5 is working well, it does a comparable job. But it’s been more prone to hiccups. I hope to see this continue with the G6. The real improvement here looks like it might be a big jump in reliability. That’s critically important if we’re going to open this CGM up to use with closed-loop systems of the future. In the few days I’ve worn it, I can say I’m more likely to dose off of the G6 than the G5, and to trust that it’s functioning as intended.
Editor’s Note: As of June 11, 2018, the Dexcom G5 is the first mobile-enabled continuous glucose system approved for Medicare patients with type 1 and type 2 diabetes.
Read Beyond Type 1’s coverage of the G6 FDA Approval and an interview with Dexcom CEO Kevin Sayer.





