My Type 1 Daughter Is In Your Care
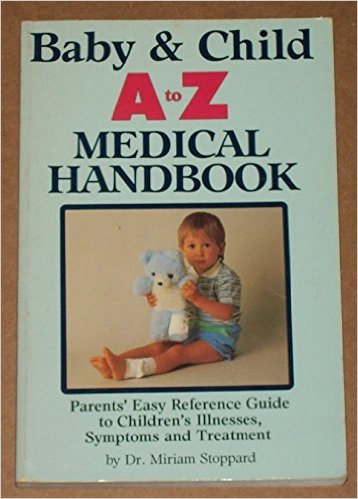 When Mary was 7 in 1998, she was diagnosed by me from this medical handbook that sat above my desk. As the personal computer and the world wide web had yet to permeate every household, I flipped through the index, looking up her “common complaints”—excessive thirst, blurry vision, headaches. After multiple possibilities, the bottom of one of the pages held an outlined box which contained the final answer: “See Also: Diabetes, page 111.” I hate this stupid book.
When Mary was 7 in 1998, she was diagnosed by me from this medical handbook that sat above my desk. As the personal computer and the world wide web had yet to permeate every household, I flipped through the index, looking up her “common complaints”—excessive thirst, blurry vision, headaches. After multiple possibilities, the bottom of one of the pages held an outlined box which contained the final answer: “See Also: Diabetes, page 111.” I hate this stupid book.
Fast forward a few months when we had emerged from the newly diagnosed fog and were venturing out into the world where other people would be tasked with monitoring Mary. From the parent driving the first grade field trip to the dance teacher to the stage manager at the community theater, there were people everywhere who were like the old me: people who knew nothing about type 1 diabetes. Not everyone had cell phones, so when the field trip left for the day, if you weren’t on the sign up sheet, you just waited anxiously for the end of the day. People still used land lines and you had to leave a number where you were going at all times and had to check in when you changed locations.
It seems so “dark ages” but, there was a simplicity in that not everything could be monitored constantly, not everyone could be reached immediately, not every fear could be wiped away with the glance at a screen. That simplicity led to simple acts, like sharing “Mary Is In Your Care” with those whom we would be handing our precious girl over to for some length of time. I would print a copy of our care document, fold it into a number 10 envelope and send it along ahead of time, or pack it in her bag and ask that she give it to the person in charge. Sometimes people would ask questions, but mostly they gulped down any anxiety, gave her a glance of kindness, tucked extra lifesavers in their pocket for her, and went about their day. We would just take a breath and have faith that all would be okay, that she would return to us safely, and thankfully, she always did.
You may have a system of your own, or a document you email to others already in place, but in case the below is helpful, it served us well from the time this photo was taken (six weeks after her diagnosis) until she left for Parsons School of Design in New York. Some details changed throughout those years—she would switch between shots and a pump several times—but it’s amazing how much has not changed. This document always gave people a basic understanding of what this amazing girl was living with, leaving them empowered to help her but not so overwhelmed they refused. For her part, Mary would hand off the envelope and skip along smiling, every inch the pure sunshine she still is today.
Feel free to use the outline below and adjust for your child’s daily care + management.
Mary Is In Your Care
DIABETES
Diabetes is the name given to disorders in which the body has trouble regulating its blood glucose, or blood sugar levels. There are two major types of diabetes: Type 1 diabetes and type 2 diabetes. Type 1 diabetes, or insulin-dependent diabetes, is a disorder of the body’s immune system—that is, its system for protecting itself from viruses, bacteria or any “foreign” substances. Scientists do not yet know exactly what causes type 1 diabetes, but they believe that autoimmune, genetic and environmental factors are involved.
Type 1 diabetes occurs when the body’s immune system attacks and destroys certain cells in the pancreas, an organ about the size of a hand that is located behind the lower part of the stomach. These cells—called beta cells—are contained, along with other types of cells, within small islands of endocrine cells called the pancreatic islets. Beta cells normally produce insulin, a hormone that helps the body move the glucose contained in food into cells throughout the body, which use it for energy. But when the beta cells are destroyed, no insulin can be produced, and the glucose stays in the blood instead, where it can cause serious damage to all the organ systems of the body.
For this reason, people with type 1 diabetes must take insulin in order to stay alive. This means undergoing multiple injections daily or having insulin delivered through an insulin pump, and testing their blood sugar by pricking their fingers for blood six or more times a day or using a continuous glucose monitor. People with diabetes must also carefully balance their food intake and their exercise to regulate their blood sugar levels, in an attempt to avoid hypoglycemic (low blood sugar) and hyperglycemic (high blood sugar) reactions, which can be life threatening. Mary was diagnosed with type 1 diabetes in November 1998.
DAILY CARE
Mary injects a dose of long-acting insulin in the morning to cover her basic body functions and then injects short-acting insulin throughout the day as needed to cover her food intake. She also balances her doses by considering stress, exercise, illness and other factors.
As referenced above, Mary must check her blood sugar throughout the day and night and make adjustments throughout to regulate her blood sugar level. This process has been simplified by a continuous blood glucose monitor that measures her blood sugar levels constantly and then transmits the data to a handheld receiver. The benefit of this device is that an alarm will sound if her number falls below 70 or rises above 200.
HIGHS AND LOWS
While the above course may sound simple, it is in fact, quite challenging. Maintaining balanced blood glucose levels is a primary and constant concern. When Mary’s blood sugar falls below 80 can she generally sense the shift. She feels shaky, has difficulty concentrating and begins to feel “fuzzy.” When this occurs, she must have quick acting sugar—such as juice. The danger would be hypoglycemia, where her blood sugar becomes so low that she loses consciousness. The protocol for an episode is to administer an emergency glucagon kit and then call 911.
Hyperglycemia, or high blood sugar, is most often identified in Mary as irritability, frustration, lack of ability to concentrate and headaches. When her number is above 200, she adjusts with insulin, exercise and fluids. There is a challenge, however, in lowering her number slowly, so as not to induce hypoglycemia. Prolonged high blood sugars can lead to diabetic ketoacidosis (DKA). The sugars lead the body to produce ketones, which are poisons, and if the body cannot rid itself of the ketones, the result is DKA. Symptoms would be flu-like. If DKA is suspected, or ketones have been identified in urine, the course of action would be to go to the emergency room. 911 should only be called if there is a lack of consciousness.
SAFETY RECOMMENDATIONS
Mary does a remarkable job of monitoring and managing her diabetes. She is responsible for 80 percent of her care and is to be commended for her responsibility, diligence and patience. In order to improve her safety, it is important that those around her know that she is a person with type 1 diabetes and be on alert for symptoms of high or low blood sugar. She must always carry emergency sugar, her kit and her Dexcom receiver. Thank you for keeping her in your care.
Read more about handing your type 1 off to a babysitter here.





