The BlueLoop System for Better T1D Management in Schools
 My daughter, Sarah, was diagnosed with type 1 diabetes January 22, 2003. I knew absolutely nothing about diabetes, so I was too naïve to be alarmed or fearful for my daughter’s future. My focus was on her immediate health needs. She spent two nights at Children’s Medical Center Dallas in Texas, and thanks to getting the insulin her body required, she began to feel much better. My first slap of reality came on the second day in the hospital.
My daughter, Sarah, was diagnosed with type 1 diabetes January 22, 2003. I knew absolutely nothing about diabetes, so I was too naïve to be alarmed or fearful for my daughter’s future. My focus was on her immediate health needs. She spent two nights at Children’s Medical Center Dallas in Texas, and thanks to getting the insulin her body required, she began to feel much better. My first slap of reality came on the second day in the hospital.
Two nurses came into Sarah’s room to test her blood sugar, which meant a finger poke. Sarah was 6 years old and started crying when she saw the lancet in the nurse’s hand. I rushed to her bedside to reassure her. “It’s okay Birdy, just one…” but then I stopped myself. What I started to say was exactly what I had said to her since she was a baby, every time she got an immunization shot, “It’s okay, just one poke and then we’re all done—no more.” But I couldn’t say that. I kept the brave face all moms of children with diabetes know too well. Once the test was over and Sarah stopped crying, I left her hospital room, found a bathroom and cried for the first time since diagnosis. Diabetes had taken away my mommy super-power to make everything better for my baby. I could make things better, but not back to how things were before diabetes. “Normal” had a new meaning for our family, and John and I were (and are) committed to making the best of our new normal.
Over the next year, we learned how to manage diabetes. Things were relatively easy when she was with us; leaving her at school was a different, scary unknown. We were blessed to have a wonderful school nurse, and I knew she would call me if there was a problem—but I still worried. I wanted to know how her day was going, what her blood sugars were and gather any observations the nurse had. I was grasping for a peace of mind. At the end of first grade, 18 months after diagnosis, I told the school nurse that over the summer, I was going to come up with a better way for us to communicate. I explained how that almost daily, I had questions for her, or wanted (needed!) reassurance about Sarah’s day. But knowing how busy she was, I didn’t call because I didn’t want to disturb her. The nurse’s eyes lit up and she said, “I have the exact same problem! I know you work full-time and I don’t want to bug you, so my non-urgent questions for you go unasked.”
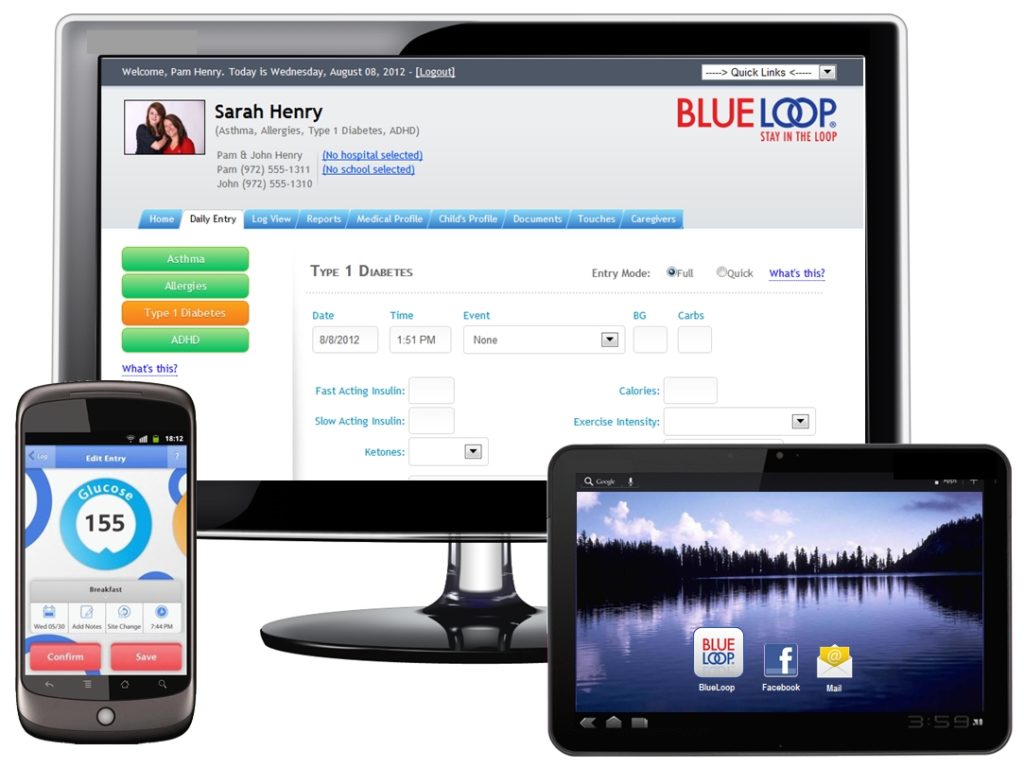
That summer of 2004, I paid a programmer $400 to program what is now called BlueLoop®. I created it for my own use—my need for a peace of mind throughout the day. The school nurse loved it and used it at least three times a day to log blood glucose (BG) tests, carbs, insulin intake, notes and to ask me questions. Within a couple months, other school nurse heard about BlueLoop and asked if they could use it, too, since they also have parents who worry about their children throughout the school day.
Early 2005, based on conversations with school nurses, and the overwhelming fear I heard from other parents, I realized I must make BlueLoop available to the diabetes community.
Fall 2008, as BlueLoop continued to grow, I gave notice to my employer of 13 years. BlueLoop needed my attention full time, even though that attentiveness meant giving up my income. All our hard work and dedication to helping others paid off in 2009. We were approached by a pharmaceutical company wanting to offer better resources to families affected by type 1 diabetes. Finally, after six years of supporting families at my own expense, someone shared our passion for helping others and was willing to support our vision with their vast resources. Over the next 30 months, with their backing, we were able to expand our reach.
Between 2012 and 2015, we expanded from 3,100 email and text message notifications per day, to over 8,000. These notifications are more than just numbers: they represent a peace of mind and better care coordination for families, schools and doctors. The pharmaceutical support ended in 2013, but we were grateful for what we learned during those 30 months. We came to realize that spreading the “good word” and making a difference in people’s lives came naturally to John and me. Our experiences with families, schools and clinics solidified our certainty that there was a need out there, and that we could fill that need.
In speaking with endocrinologists, certified diabetes educators (CDEs) and school nurses around the country, we discovered there’s a large population of underserved families we weren’t reaching. We were shown, first hand, how and why the latest cloud-based technology like continuous glucose monitors and insulin pumps never make it into the hands of low-income families. The answer: because they simply can’t afford them, which hinders care coordination among home, school and healthcare providers.
We knew BlueLoop could address the needs of these underserved families, so in 2014, we changed our business model, enabling us to make an even greater impact. We formed as a 501c3 charitable organization to provide our BlueLoop tool, education and support to others. To provide these critical resources, we started charging new families a nominal fee of $7.95 a month, while ensuring that those who couldn’t afford the cost received BlueLoop free of charge.
We all know the heavy burden type 1 diabetes places on children, families and schools, especially right after diagnosis. Both physical and emotional needs must be addressed, so John and I devoted ourselves to filling this gap. We began working more closely with clinics and schools around the country to help identify these families and provide them with the education and resources they need most—how best to care for their children while at school, educating them on best care practices and simply making ourselves available for caring exchanges and a person to call whenever they need.
Today, we find ourselves spending more time on the phone than on the computer. No technology can replace interacting directly with families and school nurses, providing education, support and a sympathetic ear. As much as we can afford to, we present at school nurse events, educating them on care coordination and the psychological impacts type 1 has on children and their families. We listen to their stories and gain a better understanding of what’s needed to improve care for our children—because that’s what matters most.
Read The Future of User-driven Design in Diabetes Devices and Tidepool—A Comprehensive Platform for Diabetes Management.





