Low Blood Sugar During Sex: Diabetes Intimacy Tips That Actually Work
Written by: Kourtney Johnson
5 minute read
June 30, 2025
A diabetes diagnosis doesn’t mean your sex life is off-limits. It’s still yours to enjoy—just keep an eye out for low blood sugar during sex. Hypoglycemia can sneak up mid-action, but with some prep and awareness, passion stays firmly in your hands.
Want to keep it sexy without crashing mid-thrust? Let’s talk lows, lust and leveling up your game.
What causes low blood sugar during sex?
Simply put, sex is exercise. It gets your heart pumping and muscles moving, which makes your body burn glucose for energy.
This can make your blood sugar drop, particularly if you take insulin or other medications that lower blood sugar
Recognizing the signs of a sexy low
Some signs of low blood sugar, like sweating, dizziness or a fast heartbeat, can feel a lot like arousal. That’s why it can be tough to tell the difference in the moment.
If you are feeling off during foreplay and/or sex, pause and check your glucose. Also, keep fast-acting carbs nearby, just in case.
How to prepare for safe, confident sex when you have diabetes
Advocates like Kesha Carter encourage people to approach sex with confidence and caution.
“Have fun and don’t stress, but at the same time make sure [your partner] knows the seriousness of the situations that may happen,” says Carter.
Here are some additional tips to help prevent lows and set yourself up for success when you are gonna do it.
Schedule your intimacy
“Spontaneous, ‘rip-each-other’s-clothes-off’ sex sounds exciting, but let’s be honest—it’s more Hollywood than real life,” says Janis Roszler, PhD, LMFT, RD, LD/N, CDCES, FAND, and author of the book Sex and Diabetes: For Him and Her. “Whether you’re managing diabetes, wrangling toddlers or juggling deadlines at work, planning intimacy helps you bring your best self, mentally and physically, to the moment.”
Eat before you get busy
A pre-sex snack can help stabilize your blood sugar. If you use an insulin pump, consider reducing your basal rate.
Use CGM trends wisely
If your continuous glucose monitor (CGM) arrow is pointing down, consider a fast acting carb snack or a pump adjustment. Talk to your provider about how to interpret trends in the context of intimacy.
Bring out the fun underwear
Roszler adds that if you know sex is on the schedule, plan ahead,
“Adjust meds if needed, have a balanced meal, maybe even bring out the fun underwear,” she says. “But most of all, look forward to the connection.”
Managing your devices: Insulin pumps + CGMs
Of course, sex with diabetes isn’t just about glucose. It’s also about gear.
“Devices in bed need to be treated like you’re avoiding the red-lasers during a bank heist,” says Carter.
Should you disconnect?
Some people choose to stay connected to their insulin pump during sex to help control blood sugar. Others disconnect for comfort or to avoid going low. There’s no one right choice—just what works best for you.
CGM Placement Tips
Be mindful of its placement. Avoid high-friction zones. Try the back of your arm, thigh or stomach to keep your CGM secure.
What about beeps and alerts?
They might interrupt the mood, but loud alerts can help you catch a low before it becomes dangerous.
And sometimes, real-life comedy says it best.
“I was always paranoid that my devices would rip off during sex,” says Sam Morrison, a comedian with type 1. “And then one time my boyfriend accidentally tore off my Omnipod in bed and he felt so guilty. Now, every time before we have sex, he very carefully checks where they are first. So, I’d recommend causing maximum guilt as soon as possible!”
Real talk from the community: Humor, snacks and survival
“PRE-treat like your orgasm depends on it,” says Carter. “If you’re trending low, maybe eat one pack of fruit snacks before and turn your CGM notifications on LOUD. Also, before getting busy, your partner should know how to treat a low blood sugar.”
Morrison adds that he always makes sure his low-blood-sugar snacks are within grabbing distance.
As for talking to your partner(s) about your diabetes, Roszler says don’t make it a big, awkward sit-down.
“A group of partners I once spoke with said they felt most at ease when they observed their loved one’s attitude toward diabetes,” says Roszler. “It wasn’t about a perfectly worded explanation. What helped them relax was seeing their partner’s comfort and confidence in managing it.
Roszler says to let explanations come up naturally. If your partner is curious and has questions, invite them to join you at your next healthcare appointment or suggest attending a diabetes education class together.
“It’s a great way to learn, connect and support each other.”
Sex with diabetes checklist: Before, during and after
✅ Snacks and fast-acting glucose nearby.
✅ CGM or Blood Glucose Meter (BGM) accessible.
✅ Humor fully stocked.
✅ Partner briefed on how to treat a low.
Own your intimacy—On your terms
Managing diabetes during intimacy isn’t about perfection. It’s about being prepared, staying flexible and having a little fun along the way.
When you feel empowered and supported, intimacy isn’t just possible—it can be incredible.

Author
Kourtney Johnson
Kourtney is a registered dietitian living with type 1 diabetes. She was inspired to study nutrition after learning about the role food plays in managing this condition. When she's not writing about all things food and diabetes-related, she enjoys reading, cooking, traveling, going to the beach and spending time with loved ones.
Related Resources
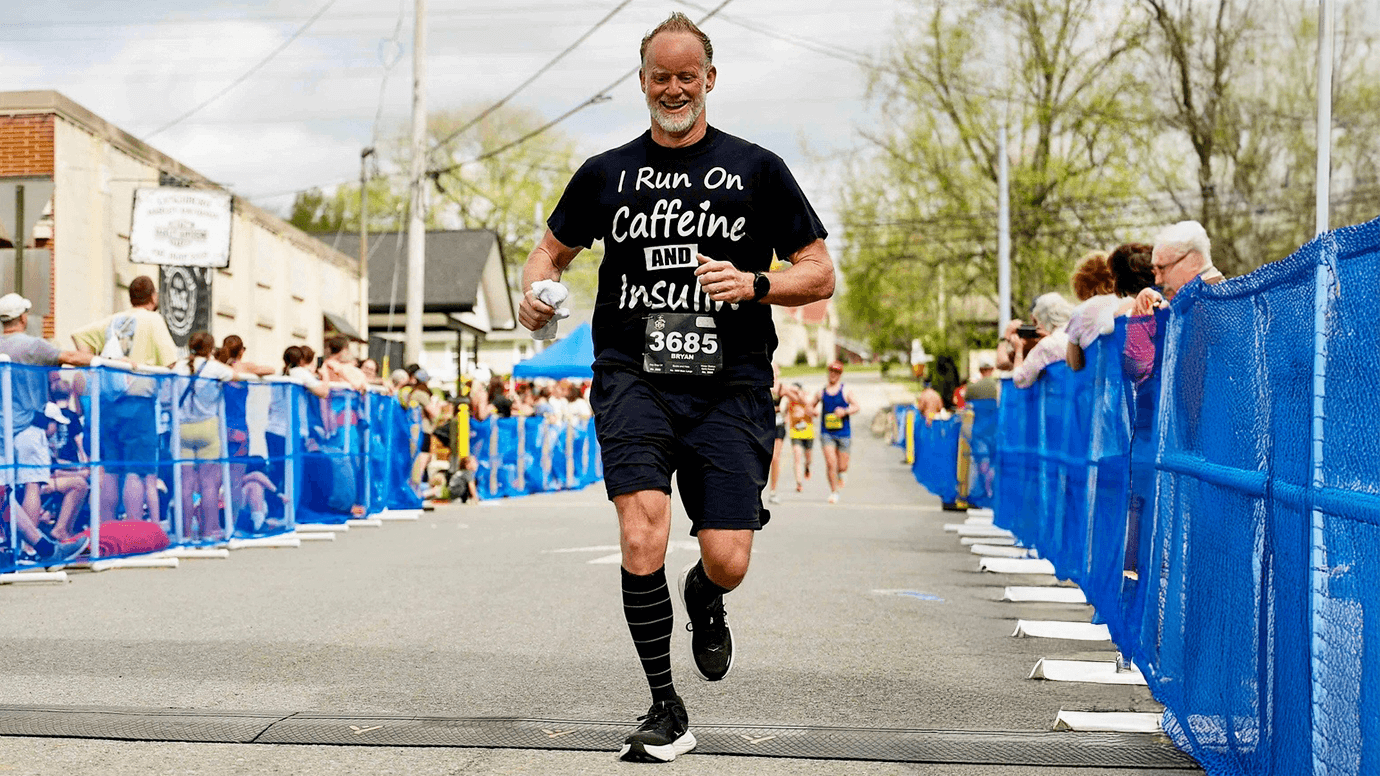
Training for a marathon takes a lot—hundreds of miles on the pavement, time and the...
Read more
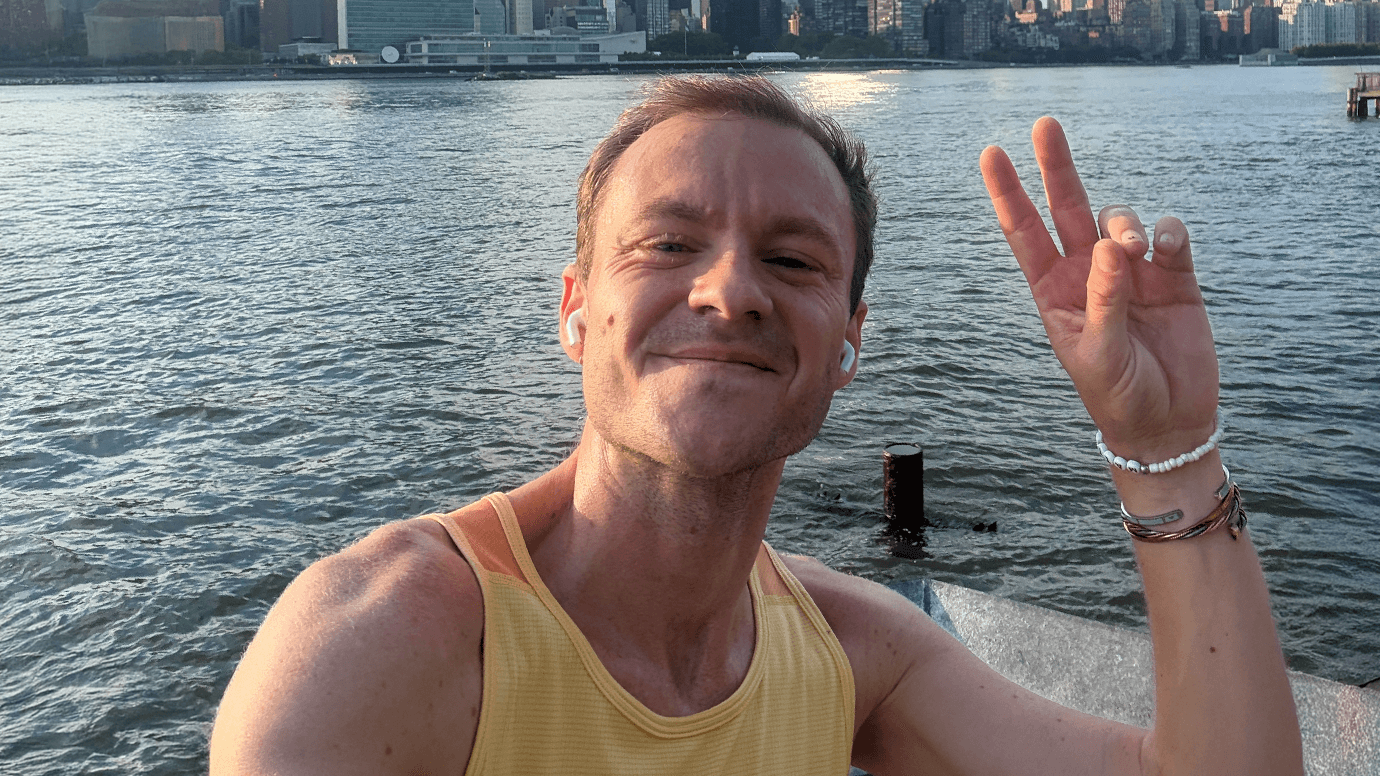
For Tanner Saunders, running isn’t just about crossing a finish line—it’s about living boldly and...
Read more
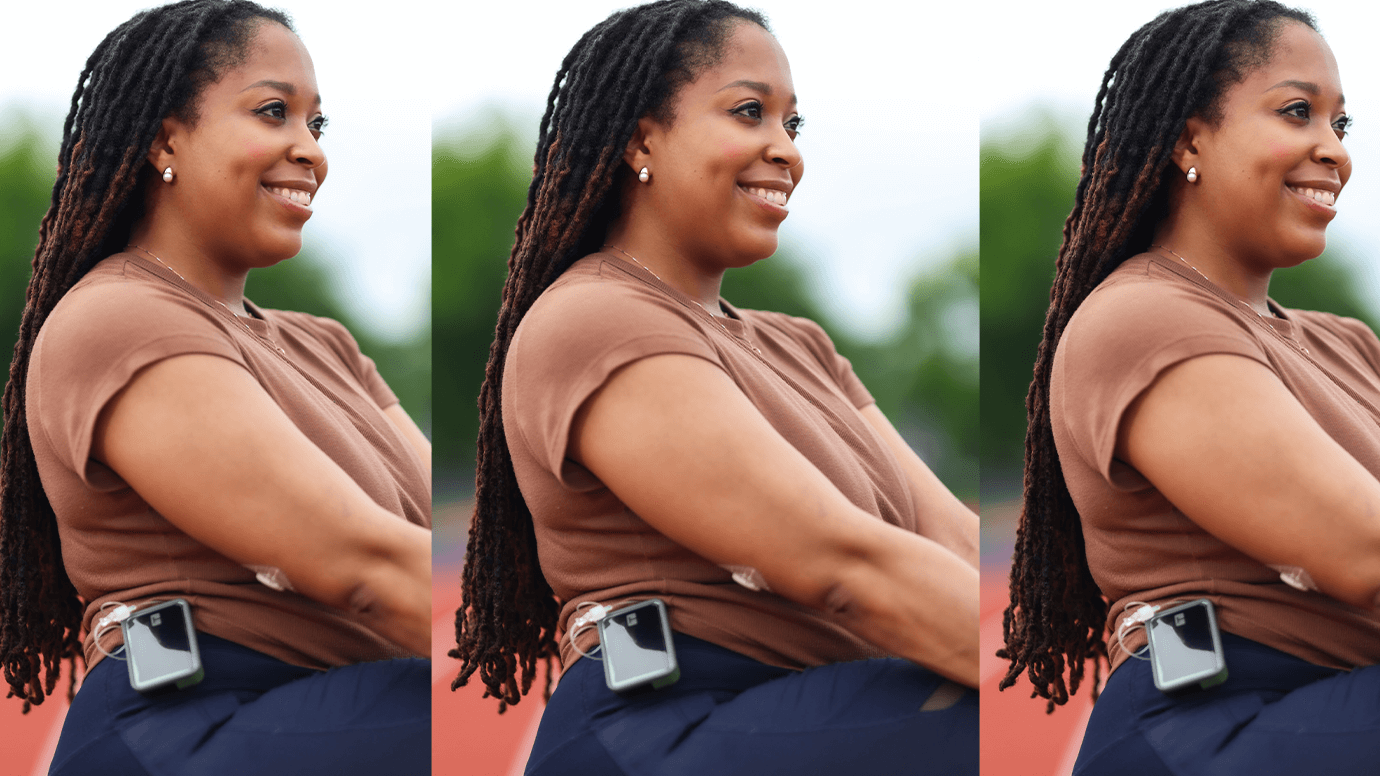
Training for a marathon takes an unimaginable number of hours—but life doesn’t hit pause. In...
Read more

