
Beyond Diagnosis
Implementation Guide
Welcome!
BT1 as a global non-profit dedicated to the diabetes community, aims to empower individuals to not just survive but thrive, uniting the diabetes community worldwide through peer support programs, global campaigns, and digital platforms.
On behalf of BT1, I extend my heartfelt gratitude to your interest in utilizing the Beyond Diagnosis toolkit, implementation guide, and learning modules. This educational resource aims to empower individuals newly diagnosed with Type 1 Diabetes (T1D) or Type 2 Diabetes (T2D) by equipping them with essential knowledge and support.
Although the toolkit can be accessed as a standalone resource for newly diagnosed individuals, you have taken steps to support your community by offering your expertise in guiding people with diabetes through each section.
We know that the foundational concepts of diabetes education can be implemented in any community, yet understand and appreciate that your community is unique. At BT1, our commitment to health equity lies at the core of this program. We strive to provide accessible, culturally sensitive education to ensure that everyone receives the support they deserve, regardless of their background. Your partnership in this endeavor will significantly enhance our reach and empower individuals to navigate their diabetes journey with confidence.
Sincerely,
Melanie Batchelor, MHS, RD, LDN, CDCES
Social Impact Manager, Science Advisory, Community Education, and Content
Beyond Type 1

Introduction
BT1 recognizes that being diagnosed with diabetes can be an overwhelming experience, understanding the daunting learning curve that comes with it. That’s why Beyond Diagnosis serves as your partner in this diabetes journey, helping individuals transition from uncertainty to confidence with a resounding “I got this.” This five-part education program is tailored for individuals over 18, offering tools, encouragement, and a support system to navigate the complexities of diabetes management.
Beyond Diagnosis focuses on three main pillars:
- Survive: Early and accurate diagnosis of diabetes can save lives. Diabetes education, often termed survival diabetes education, is vital for individuals recently diagnosed.
- Thrive: Education can delay the onset of complications and significantly improve quality of life.
- Drive: Our program is designed to translate clinical diabetes terminology into practical, understandable language. It aims to be accessible and applicable to all, particularly targeting minorities and underserved populations.
How to Use This Implementation Guide
The primary objective of this implementation guide is to aid instructors in effectively utilizing the program materials for individuals with T1D and/or T2D. It will provide detailed instructions for conducting educational sessions on diabetes management and utilize the Beyond Diagnosis toolkit for teaching purposes. Each section provides the instructor with an overview of the diabetes education topic, an outline with essential teaching points (which correspond to the T1D and T2D toolkits), engaging group activities, and reflection prompts. Essentially, this implementation guide serves as the foundation for delivering each educational session and applying the toolkit’s teachings. Please be aware that the needs of individuals with diabetes are diverse, and your efforts to align the curriculum with your community’s needs and interests will greatly enhance the experience for your participants.
Understanding Diabetes Education
What is diabetes education?
Diabetes education or diabetes self-management education (DSME) is the process of providing knowledge, skill and ability necessary for diabetes self-care. Now, diabetes self-care refers to the series of behavioral practices to manage diabetes. There are a wide range of behaviors that can help a person with diabetes live healthfully such as healthy coping, healthy eating, being active, taking medications, monitoring, reducing risks, and problem solving.
The responsibility for managing diabetes falls on people living with the condition and their families. This can be overwhelming, especially when guidance and support are lacking. It has been demonstrated that continuous diabetes education is a fundamental tool right after diagnosis and also on an ongoing basis to support the individual with diabetes in living their healthiest life and minimizing health issues that can be caused by diabetes.
When is diabetes education needed?
According to the American Diabetes Association (ADA) , there are four critical times when people should be referred to a Diabetes Self-Management Education:
- At diagnosis: This initial education equips individuals with the necessary foundation for managing their condition effectively, including understanding insulin therapy, blood glucose monitoring, healthy eating, and preventing complications.
- Annually: Regular education sessions ensure individuals stay updated on the latest advancements in diabetes management, address any evolving challenges, and refine their self-care skills.
- When complicating factors emerge: Early education about kidney disease, heart disease, eye disease, nerve disease, and emotional distress can empower individuals to adopt preventive measures and positively influence self-management behaviors.
- When transitions in life occur: Life changes like starting a new job, getting married, or having children can disrupt established routines and require adjustments to diabetes management strategies. Education empowers individuals to navigate these transitions seamlessly and with supportA.
The Association of Diabetes Care and Education Specialists (ADCES) recommends that diabetes education should be an ongoing process. Continuous learning empowers adults with diabetes to:
- Improve their health outcomes: Studies have shown that DSME can lead to better blood glucose control (HbA1c), reduced risk of complications, and improved overall quality of life.
- Increase self-confidence and problem-solving skills: With ongoing education, individuals become more confident in managing their diabetes and can effectively address challenges that arise.
- Adapt to changing circumstances: As circumstances and treatment options evolve, continuous education helps individuals adapt their self-care strategies to maintain optimal health.
Why is diabetes education and diabetes self-management important?
Diabetes education is not just a one-time event but a continuous process for adults with diabetes. By receiving ongoing education, individuals can gain the knowledge, confidence, and skills needed to manage their diabetes effectively, improve their health outcomes, and live a fulfilling, healthy life. Individuals in your community rely on your continued support to assist their journey with diabetes!
Diabetes education is an essential component of diabetes care that can influence diabetes management self-efficacy and help prevent or delay long-term health effects that can be caused by diabetes.These interventions can also address the social determinants of health that contribute to higher diabetes rates in underserved communities, promoting health equity and well-being for all. Diabetes education brings us one step closer to improving health disparities in communities significantly impacted by diabetes and honoring the American Diabetes Association’s Health Equity Bill of Rights:
- The right to access insulin and all other drugs affordably.
- The right to healthy food.
- The right to insurance that covers diabetes management and futures cures.
- The right to not face stigma or discrimination.
- The right to avoid preventable amputations.
- The right to participate in clinical trials without fear.
- The right to stop prediabetes from becoming diabetes.
- The right to a built environment that does not put you at higher risk for developing diabetes
- The right to the latest medical advances.
- The right to have your voice heard.
Understanding Your Audience
What are effective teaching principles for diabetes education?
Understanding the essentials of adult learning is crucial for effective diabetes education interventions. Tailoring your diabetes education sessions to your audience will help them apply the information to their personal experiences, which improves overall learning. Strong educators adapt their diabetes education instructional delivery methods to the needs of their learners. Please use this implementation guide and toolkit as an effective framework that can be personalized to your community’s needs.
What are my community’s learning needs?
By considering factors like learning styles, cultural backgrounds, and varying levels of existing knowledge, educators can create engaging and accessible learning experiences. This, in turn, promotes better information retention, empowers individuals with diabetes to make informed decisions about their health, and ultimately leads to improved self-management outcomes.
When considering personalizing your diabetes education program to meet the needs of your community, consider:
- Age
- Gender
- Cultural background
- Educational level
- Preferred language including needs for translations, sub-titles, or interpreters
- Preferred method of learning (visuals, stories, hands-on activities, videos, presentations, discussions, journaling, and action planning to enhance engagement, etc)
- Location where the community feels most comfortable learning
- Time of day most convenient for community learning to occur
- Barriers to attendance like transportation, internet access, and/or childcare
- Feasibility of group education format or 1:1 format
- Space constraints for inclusion of support persons (spouse, partner, child, etc)
- Health topics of interest to your community
- Frequent misconceptions about health in your community
- Real-life examples that can resonate with your community (recipes, stories, guests, etc)
- Finding one small way to demonstrate to participants that you care about the individuals in your group
How can I provide meaningful learning?
Meaningful learning occurs when new knowledge is linked to a person’s experiences and interests. Meaningful learning is learning more easily retained because it relates to real-life scenarios of the learner. This type of learning is linked to the priorities and values of each person. As a community educator, your role is KEY in tailoring diabetes education guidance to the group’s individual experiences. This key strategy will improve the total impact your education has within your education sessions and within your community.
What is person-centered diabetes education (PCDE) and how can it be used within diabetes education?
William Polonsky PhD, a leading diabetes psychologist, has championed the importance of addressing the real-life challenges of living with diabetes. His approach provides mental health support to individuals with diabetes and their families, which often are unnoticed and unaddressed in traditional care settings and approaches.E He states, “PCDE respects the patient’s autonomy, acknowledges their unique experiences, and builds upon their existing strengths.”
Using Dr. Polonsky’s approach to foster a collaborative partnership between yourself as the instructor and your group as the individuals living with diabetes will lead to more effective diabetes management. Adopting a supportive and empowering tone for delivery is highly recommended as the best practice for delivering diabetes education and self-management guidance.
How can I provide diabetes education and guidance in a supportive manner?
How we talk about diabetes and foster supportive diabetes care environments is essential to the Beyond Diagnosis programs. We have built the Beyond Diagnosis programs using this philosophy and supportive diabetes language to foster a positive discussion and experience for participants. As you begin this education series in your community, take some time to ensure your approach is fully aligned with the best practices in speaking the language of diabetes in a supportive way.
Best practices for communicating about diabetes include “use language that:
- Is neutral, non-judgmental, and based on facts, actions and physiology/biology
- Is free from stigma
- Is strengths-based, respectful, inclusive, and imparts hope
- Fosters collaboration between patients and health care professionals
- Is person-centered.”
Click here to learn more!
Breaking Down Each Section
The Beyond Diagnosis Implementation Guide is designed to be delivered in five (5) sections. We recommend hosting four, 90 minute group sessions, and one 60 minute final virtual session. Each section of this program is organized around core topics aimed at thoroughly addressing the needs of participants living with diabetes and has been designed to give you an easy template to follow as you facilitate the educational session, including:
1. Decoding Diabetes (90 minutes)
This section discusses how diabetes affects the body’s physiology, what insulin is and how it works, and the treatments that are effective for managing blood glucose in T1D and T2D. Participants will explore the unique characteristics and challenges of diabetes from participants who live with T1D and T2D themselves. Your community will learn to Identify the most common symptoms and underlying causes of both T1D and T2D. Lastly, the group will learn about the different types of diabetes medications available and their essential roles in diabetes management.
SPECIAL NOTE: Be aware that misdiagnosis of diabetes can occur due to overlapping symptoms with other conditions or atypical presentations. Inaccurate generalizations regarding diabetes diagnosis are prevalent in health care settings (ie, individuals with weight above the healthy range can be assumed to have T2D), and it is not uncommon that specific diabetes diagnostic tests can be skipped. Understanding the correct diagnosis of diabetes is essential in providing individuals with a strong foundation of their diagnosis and what treatments are available to them. See this resource for ways to definitely determine proper diagnosis.
2. Creating Your Best Path Forward (90 minutes)
This section focuses on strategies for managing blood glucose levels effectively, including monitoring techniques and lifestyle adjustments. Participants will also learn how to recognize, prevent, and manage episodes of hypoglycemia and hyperglycemia.
3. Fuel Well to Feel Well & Move Your Body (90 minutes)
Here, participants will receive guidance on the importance of physical activity and exercise tailored for T1D. They will also learn about nutrition choices and meal planning strategies to support optimal diabetes management.
4. Building Your Diabetes Support Team (90 minutes)
This section highlights the significance of assembling a comprehensive healthcare team for diabetes care. Participants will learn about the roles of different healthcare professionals in their diabetes management. Additionally, strategies for managing the emotional and psychological aspects of living with diabetes will be discussed, emphasizing the importance of mental well-being.
5. Tap into A Community & Thrive Together (60 minutes- virtually or as a support group)
The final section emphasizes the importance of community support in thriving with diabetes. Participants will be provided with resources to connect with others living with diabetes, fostering a sense of solidarity and mutual support. This section underlines the significance of community in the journey of managing diabetes effectively.
Promoting Your Program
Email Invitation
Promoting the Beyond Diagnosis program with your potential participants is key to reaching those who can benefit most. Below we have included an email template you may find helpful when inviting people to attend your education offerings, whether they be virtual or in-person.
Hi [Patient Name],
Getting diagnosed with diabetes can feel like a lot. Let’s work together to get from “I can’t do this” to “I’ve got this.” Diabetes will have its challenging days, but you’ll be prepared with the knowledge, tools, understanding and—most importantly—the community to support you.
Join me for a journey Beyond Diagnosis, a resource created by Beyond Type 1, a nonprofit committed to helping people not just survive but thrive with diabetes.
We’ll talk through things like:
[Adjust based on your session focus]
- What diabetes is and what’s going on in the body
- How food, movement, and blood sugar connect
- Tips for making a care plan work in real life
- Emotional health and where to turn for support
The Beyond Diagnosis program provides easy to understand diabetes education in a fun and interactive way. You’ll get a printed or digital guide, and we’ll walk through it together.
[Insert session details – date, time, location or link]
Let me know if you have any questions or if there’s anything you’d like to talk through ahead of time. Hope to see you there.
P.S. Finding your people is part of diabetes care, too. Follow @beyondtype1 to connect with others who get it.
Program Evaluation
Assessing the knowledge, behavior change, and sense of confidence of your program participants is key.
Instructions
Have your participants answer the 5 simple questions below using the answer scale for each question. You will be able to quickly compare the pre survey responses to the post survey responses to determine the effectiveness of your program.
Recommended Questions
- I have access to education materials that are easy to understand.
- I have participated in a diabetes education program that was really helpful.
- I have the skills that I need to manage my diabetes.
- I feel really confident managing my own diabetes.
- I’d definitely recommend a diabetes education program to other people with diabetes.
Recommended Answer Scale
- Strongly Agree
- Agree
- Neutral
- Disagree
- Strongly Disagree
Sharing Successes with Beyond Type 1
We want to hear from you! Share how beneficial the Beyond Diagnosis resources have been for you and your community. Simply email [email protected] with any feedback you have.

Section 1
Decoding Diabetes
Instructors can seamlessly present the lesson using the corresponding BT1 Decoding Diabetes presentation (with speakers notes) and the BT1 and BT2 toolkits Decoding Diabetes section (p, 3-18 for T1D Toolkit and p. 3-16 for T2D toolkit) . The participants’ toolkits include engaging visuals, diabetes ambassadors, and educational resources which correspond with your instructor slides and speaking notes. Let’s get started!
Introduction Tips
- Welcome and program overview: Briefly introduce yourself, the program, and the learning objectives for the session.
- Encourage participants to introduce themselves: Build camaraderie within your group through introductions.
- Make a list of the group’s curiosities: Encourage each person to share one thing they hope to learn in today’s session. Record each participant’s learning objective so each item can be addressed during the education session.
- Materials distribution: Ensure all participants have a copy of the Beyond Diagnosis toolkit. Today’s session will cover the Decoding Diabetes section within the toolkits (p, 3-18 for T1D Toolkit and p. 3-16 for T2D toolkit)
- Introduce your group to the Beyond Diagnosis ambassadors for Decoding Diabetes.
Education
Diabetes: What Is it?
Diabetes happens when the body stops producing insulin—or using it properly. Insulin is a hormone produced by the pancreas that helps manage the level of glucose in the blood and transform glucose into energy. When insulin isn’t produced—or doesn’t work well—it leads to unhealthy blood sugar levels and low energy.
What is T1D?
Having T1D means your body cannot make its own insulin. T1D happens when the immune system attacks the beta cells in the pancreas. Beta cells are the cells that make insulin. This autoimmune attack on these beta cells is so aggressive that the body of a person with T1D loses its ability to make insulin. Because people with T1D can no longer make insulin on their own, they must get insulin from an outside source. Taking insulin is not “optional” if you live with T1D. A person with T1D will need to take insulin from the moment they are diagnosed. For a person with T1D, having access to insulin is of the essence.
What is T2D?
If you have T2D you still make some insulin but either not enough or your body doesn’t use it correctly. This can be known as “insulin resistance.” T2D can go undetected for many people because the symptoms are more mild and develop progressively over time, but that doesn’t mean taking care of T2D is any less important. There are many effective treatments for T2D, and we will learn about some of them today. T2D is far more common and in the USA, at least 8.6 million people live with T2D but are undiagnosed.
What are the most common symptoms of diabetes?
- Being Thirsty all the time
- The need to pee too frequently
- You’re just exhausted!
- Losing weight and don’t know why (T1D only)
What causes T1D and T2D?
T1D
Research is still ongoing to determine the cause of T1D. Current thinking suggests that there is a combination of environmental and genetic factors that contribute to T1D diagnosis.
There are multiple stages of T1D.
- Stage 1: The individual has two or more autoantibodies but still has normal blood glucose levels and no symptoms of T1D.
- Stage 2: During this stage, people will experience higher blood glucose levels—but may not be experiencing symptoms at this stage.
- Stage 3: This is the classic stage where most people receive their T1D diagnosis. At this stage, people with T1D lose their ability to produce their own insulin—resulting in high blood glucose levels and the classic symptoms of T1D.
Today, T1D is most often diagnosed in the final stage (stage 3), when symptoms become present. However ongoing research and T1D screening efforts are now able to capture individuals who are likely to develop T1D, offering effective treatment to delay their progression towards T1D.
Autoantibody screening for T1D should be recommended to individuals with a family history of T1D, younger age at diagnosis, unexplained weight loss, and shorter time to insulin treatment.B It is important to note that even adults diagnosed with diabetes or those with body weights above the healthy range should still be considered for autoantibody testing to confirm or rule out the diagnosis of T1D, because T1D can occur at any age or in any body size.
T2D
Insulin resistance has an important role in the development of T2D. Insulin resistance means that the pancreas still produces insulin, but the body progressively becomes less sensitive to it, which causes increased blood glucose levels. As the body becomes less sensitive to insulin, the pancreas begins to produce more and more to help cells access the insulin they need to create energy. Over time the pancreas struggles to keep up with the increased demand for insulin as the body progressively loses its sensitivity to the body’s insulin. The pancreas eventually cannot keep up with the body’s increased demand for insulin because the insulin-producing cells (beta cells) are too fatigued from overproduction resulting in high blood glucose.
It’s very important to understand T2D is not limited to only people who have higher body weight . This is a common misconception about T2D. While the majority of those with T2D also experience higher body weight, T2D can affect people of all sizes and backgrounds. Most importantly, having T2D does not mean you have failed in any way. There are many misconceptions and stigmas about diabetes which can make taking care of it even more difficult.
T2D is the most common form of diabetes and can result from a wide range of lifestyle and genetic reasons. Worldwide, about half of those living with T2D are not diagnosed and In the U.S., at least 8.6 million people live with T2D but do not know it (CDC). T2D diagnoses are frequently associated with lifestyle factors, including poor diet, high blood pressure, obesity, physical inactivity, taking certain medications and genetics. Underserved communities face additional challenges in developing T2D such as not having access to safe places to exercise or having affordable, convenient access to fresh and nutritious food.
Adults and children are screened for risk for T2D at regular intervals within healthcare settings, but this may not identify risk or help diagnose T2D in all cases. Individuals with someone who has T2D within their family are much more likely to develop T2D themselves because the genetic link is very strong, but poorly understood in research.
Additional risk factors for developing T2D are:
- Age (greater than 35)
- Men are more likely than women to have undiagnosed diabetes
- Taking medications that can increase risk for diabetes like glucocorticoids, statins, thiazide diuretics, some
- HIV medications, some antipsychotic medications, protease inhibitors, nucleoside/nucleotide reverse transcriptase inhibitors,
- Diagnosis of HIV (having HIV and taking some HIV medications can both increase the risk)
- Prior gestational diabetes
- Polycystic ovarian syndromeB
The good news is that if T2D is adequately managed, it is possible to live a full life. Insulin resistance is responsive to many healthy lifestyle habits such as physical activity, medications, and other forms of self-care. To manage your blood glucose, you don’t need to manage T2D, you don’t need to do anything drastic. T2D isn’t a one-size-fits-all condition. The way it affects you won’t be the same way it affects another person with T2D. However it is still important that you find a T2D management regimen that works for your life to keep you healthy.
Take a moment to engage your audience with trivia
Diabetes Diagnosis Trivia
- T1D is more common than T2D.
- FALSE; T2D represents 90-95% of cases.
- T2D can be prevented or put into remission with lifestyle changes.
- TRUE; Lifestyle approaches are effective at managing T2D. T1D can primarily only be treated by lifelong insulin therapy at this time.
- T1D and T2D can impact people of all ages.
- TRUE; Previously, it was thought that T1D could only be diagnosed in children, but we know this is no longer true. T2D was thought to only impact adults, but it is now being diagnosed in children and adolescence, too.
- T1D requires insulin therapy but T2D may take other medications that aren’t insulin to manage their blood glucose
- TRUE; The best treatment for T1D is insulin. There are different medication options for managing T2D which can include insulin at some point.
- Risk factors that increase your chances of T2D are lifestyle, race, and genetics
- TRUE; Most risk factors for T2D are genetic (race, sex, family medical history of T2D) but can also include lifestyle behaviors like inactivity or poor diet.
- It is still possible to live a long and healthy life with diabetes.
- TRUE; Many treatments are available for diabetes. Living a healthy lifestyle and managing your glucose is possible!
What treatments can help manage diabetes?
The treatments for T1D and T2D differ, but there are many strategies that are effective for both. These include the core self-management principles: healthy eating, being active, healthy coping, taking medication, monitoring, problem-solving, and reducing risks. These daily health behaviors are essential for long-term health and wellness for all adults, especially those with diabetes. Choosing balanced meals/snacks, staying active and moving your body, managing stress, taking medications, and keeping in close contact are essential health lifestyle habits regardless of which type of diabetes you have.
Lifestyle Approaches |
Description |
T1D? |
T2D? |
| Healthy Eating Plan | Making nutritious food choices and developing balanced meals for optimal health. | ✕ | ✕ |
| Active Lifestyle | Incorporating physical activity into daily routines in a consistent way that you enjoy. | ✕ | ✕ |
| Glucose Monitoring | Regularly checking glucose to understand patterns and identify changes. | ✕ | ✕ |
| Healthy Coping | Identifying and managing emotional aspects of living with diabetes and developing strategies to manage stress and maintain a positive outlook | ✕ | ✕ |
| Taking Medications | Adhering to your diabetes medication treatment plan, including taking your medications as prescribed on a daily basis. | ✕ | ✕ |
| Reducing Risks | Staying on top of routine health care visits with your health care team to ensure long-term health of body systems that can be impacted by diabetes such as: eyes, kidneys, nerves, stomach, teeth, reproductive organs, and feet. | ✕ | ✕ |
| Problem Solving | Identifying and addressing challenges that arise during the course of managing diabetes. This can be done independently and/or in coordination with your health care team. | ✕ | ✕ |
What should I know about diabetes medications?
- Each participant’s health care team will recommend the medication regimen that is best. However, it’s helpful for each person to understand how your medications work and what options are available.
- In T1D, taking insulin is imperative to keeping blood glucose in a healthy range. Many people do not realize that there are different kinds of insulin they can try and different ways they can be administered (ie, syringe, insulin pen, insulin pump, auto-injector, and inhaler). Learn more about the insulin you take, how it works, and make sure to ask questions about the insulin. The important part is to find the option that works best for your lifestyle and to keep glucose in a target range. Lifestyle behaviors we have discussed are still incredibly important in managing T1D.
- In T2D there are even more medication options! These are additional tools that support key body functions and combat insulin resistance and high blood sugars. Some of the medications are pills and others are injectable. If participants take more than one pill to help manage their diabetes each day, it may be possible to have the diabetes medications combined into one pill for convenience, improving medication adherence. For those who may not have reached their glucose goals yet, encourage them to contact their healthcare team for a medication adjustment or to consider adding more medication. It’s important to understand that needing more medication to manage T2D is normal since the pancreas progressively gets more tired from trying to manage the body’s increased glucose levels over time. This is the progressive state of T2D, not a reflection of effort or failure on behalf of the person living with T2D! Medication regimens are important because they keep blood sugars in a healthy range, which is what preserves health and protects the body systems from the impact of high glucose levels.
Non-Insulin Medication Options |
|||
|---|---|---|---|
Category |
Names |
Action |
Delivery Method |
| Biguanide | Metformin | Limit glucose produced by liver | Pill |
| Sulfonylureas | Glipizide
Glimepiride Glyburide |
Encourage pancreas to produce more insulin | Pill |
| Dipeptidyl Peptidase-4 (DPP-4) Inhibitors | Sitagliptin
Saxagliptin |
Increase insulin production when glucose is elevated, reduce glucagon production when glucose is stable, and slows digestion | Pill |
| Glucagon‐like peptide‐1 (GLP-1) Receptor Agonists AND
Dual Action Gastric Inhibitory Polypeptide (GIP) and GLP‐1 Receptor Co-Agonists |
Liraglutide
Semaglutaide |
Stimulate intestinal hormones that increase insulin production | Pill
Non-insulin injection |
| Sodium-Glucose Cotransporter-2 (SGLT2) Inhibitors | Canagliflozin
Dapagliflozin Empagliflozin |
Help kidneys excrete more urine to reduce blood glucose | Pill |
| Thiazolidinediones (TZDs) | Pioglitizone
Rosiglitazone |
Improve insulin sensitivity in the muscle and adipose tissue | Pill |
| Meglitinides | Repaglinide
Nateglinide |
Increase insulin production | Pill |
*Note: These medications are commonly prescribed for the management of T2D. Insulin is the required treatment for T1D. Information about insulin can be found in the “Insulin Options” table above.
Insulin Options |
|||
|---|---|---|---|
Category |
Names |
Action |
Delivery Methods |
| Ultra-rapid acting | Fiasp or Apidra | Designed to be taken shortly before meals to help manage blood sugar spikes that occur after eating | Syringe
Insulin pen Disposable insulin pen cartridge Insulin pump |
| Inhaled | Affrezza | Designed to be taken shortly before meals to help manage blood sugar spikes that occur after eating | Disposable inhaled insulin cartridges |
| Rapid-acting | Novolog, Fiasp, Humalog, Apidra, asaprt (generic), lispro (generic) | Designed to be taken shortly before meals to help manage blood sugar spikes that occur after eating | Syringe
Insulin pen Disposable insulin pen cartridge Insulin pump |
| Short-acting | Humulin R, Novolin R | Designed to be taken 30-60 minutes before meals to help manage blood sugar spikes that occur after eating | Syringe
Insulin pen |
| Intermediate-acting | NPH, Humulin N, Novolin N | They are often used in combination with rapid- or short-acting insulins to manage blood glucose levels throughout the day and night. Has an onset of 1-2 hours, a peak effect at 4-12 hours, and a duration of 12-18 hours | Syringe
Insulin pen |
| Long-acting | Lantus, Basalgar, Semglee, Levemir, glargine (generic), detemir (generic) | They are designed to provide a steady level of insulin throughout the day and night. Long-acting insulins typically have an onset of 1-2 hours, no distinct peak, and a duration of up to 24 hours | Syringe
Insulin pen |
| Ultra-long acting | Tresiba, toujeo | They are designed to provide a steady level of insulin throughout the day and night. They have the longest duration lasting more than 24 and up to 42 hours. | Syringe
Insulin pen |
| Premixed | Humulin 70/30
Novolin 70/30 Humalog Mix 50/50 Humalog Mix 75/25 Novolog Mix 70/30 |
Premixed insulins combine rapid-acting or short-acting insulin with intermediate-acting insulins reducing the number of injections needed per day. These formulations contain meal time and long-acting insulin within one injection. | Syringe
Insulin pen |
*Note: Insulin is required for management of T1D. Insulin can also be used to manage T2D, but is most commonly combined with other non-insulin medications like diabetes pills.
What Methods Can Be Used to Deliver Insulin?
Vial and Syringe
Draw up insulin from a small bottle (vial) through the needle and into a syringe.
Insulin Pen (disposable)*
Insulin pens that are disposable are filled with insulin and can be discarded once all of insulin has been used. They look like a writing pen but have a syringe as the point (instead of ballpoint with ink). They come in boxes with multiple disposable insulin pens. Some insulin pens have memory features to remember doses, calculate doses, or provide reports to your health care team.
Insulin Pen (replaceable insulin cartridge)
Some insulin pens use replaceable cartridges. These devices help reduce waste by re-using the insulin pen component and only replacing the insulin cartridge once the insulin is used or expired. Some insulin pens have memory features to remember doses, calculate doses, or provide reports to your health care team.
Inhaler
This type of insulin is inhaled through the mouth and delivered to the body through the lungs via a dry powder insulin. It is similar to using an inhaler for asthma, but a different shape.
Jet Injector
This needle-free device injects insulin under the skin using a spring-loaded mechanism that releases the dose under the skin. Jet injectors can be helpful for those who have difficulty with injecting themselves or have variable insulin absorption.
Pump (tubed or tubeless)
Insulin pumps are small devices that deliver personalized doses of insulin throughout the day.Traditional insulin pumps are worn outside your body (eg, pager on your belt or in a pocket). There is a plastic tube which connects to a cannula (small plastic or metal needle) which delivers insulin under your skin. A person wearing an insulin pump needs to independently change the infusion sites every few days. Patch-style insulin pumps do not have tubing and instead attach directly to your skin with adhesive and deliver insulin under your skin using a hand-held controller.
Artificial Pancreas (Automated Insulin Delivery)
AID systems combine an insulin pump, a continuous glucose monitor, and a diabetes program (algorithm) to deliver insulin and adjust the amount based on the person’s glucose trends. All pumps on the market offer some form of AID.
*Disposable insulin pens are the most common way to administer insulin in the USA.
Where should I inject my diabetes medicine?
- Insulin and other medications injected to manage blood sugars can be injected in many different locations in the body. The goal is to inject the insulin into the fat layer just beneath the skin as this is where insulin is best absorbed. Below are some locations where injectable medications for diabetes can be injected. Encourage participants to choose a location that they can see, access, and reach with ease.
- Rotation of injection sites helps keep your skin healthy. Avoid taking your injection in the same location repeatedly as this can harm your skin or interfere with how your medication is absorbed. When you take injectable medications for your diabetes, rotating your injection sites (see below) will keep your skin healthy and your medication working properly. If you have questions or concerns about your injection sites, contact your health care team to examine your skin.
Diabetes Injection Know-How
- Those with T1D need to take insulin every day (multiple times per day) or use an insulin pump to stay healthy. Those with T2D also need to take their medications every day as prescribed by their doctor, but the medication may or may not be insulin.
- Insulin is essential for survival in T1D Taking diabetes medication is important for all who live with diabetes and keeps your blood glucose in a healthy range.
- Work with your healthcare team to determine the type of medications that are right for you. Don’t be afraid to try different options until you find the diabetes medications that work best for you, your blood glucose , and your lifestyle.

Optional Learning Activity
The instructor may demonstrate the correct insulin injection technique and disposal and allow each participant to practice the technique (if appropriate). This learning activity is recommended if you have group participants who are using injectable medications like insulin, but may not be necessary group activity if the participants do not require injectable medications. Here are the steps:
- Choose a clean spot on your skin that you can easily see and reach.
- Insert the needle straight in at a 90-degree angle.
- Push the insulin in all the way. If you’re using a syringe, keep the needle in for 5 seconds; for pens hold it for 10 seconds.
- Take the needle out at the same angle you put it in.
- Press on the spot to stop any leaks.
- Always throw away used needles safely to avoid accidents. Use a special container for sharps, like a thick plastic bottle (ie, sharps container, laundry detergent or dishwasher pod container), and follow the local rules for disposal.
Group discussion
- What are some other challenges that can make taking diabetes medications difficult?
- What are some things you have tried that make it EASIER to take your diabetes medication?
- What is something you wish you would have known when you first started taking medication for your diabetes?
Peer Tips
Do you have fears about taking insulin injections? If you are nervous about insulin injections, do not be afraid to ask for help from family members, your doctor, or a mental health specialist. Remember, it’s normal to feel uneasy about injecting insulin at first. Allow yourself some time to get used to the new routine, and think about practicing on an orange to gain comfort with it. With practice and patience, you’ll become more comfortable over time. Most importantly, stick with it! Here is advice from people who live with diabetes:
“No matter what kind of diabetes you have, insulin is just a tool. Having to use—or not use—insulin is not a reflection of your morality. It doesn’t make you a good or bad person…Insulin is just another tool available to us, and thank God because it’s amazing!”
Rachel Lalonde (T1D)
“If you’re newly diagnosed, I would say maybe try injections.. I remember there were a few friends that told me that whenever they were first meeting their diabetes educator, they would practice on fruit and things like that. It’s like your skin, so you can get a feel for how much to push down or how it feels physically in your hand. And if you absolutely can’t do injections, try a pump. Obviously, it’s not always the easiest thing with accessibility and affordability, but as long as you’re getting your insulin and what you need for your management in some way or another, that’s what matters.”
Damarius Palacios (T1D)
“When I first found out I had T2D, I was furious and so scared for what would happen next. I was so scared watching my numbers be high and not knowing what I should do about it. I was afraid the medication wasn’t working and that I would need more medication. I was so overwhelmed thinking about eating well and exercising each day that it was easier to not do any of it.
I’ve learned that it’s okay to feel that way, angry at diabetes. But, that it’s important to still take care of myself. Finding my community of friends to support me and help me understand what worked for them was helpful. Someone even helped me find a caring doctor, which helped me get the right medications and finally start feeling better again. I don’t have to worry now about my numbers because they’re great, and I know what to do if that changes. I am in control again!”
Jane Doe (T2D)
“Everyone in my family had diabetes, so I wasn’t surprised when it happened to me, too. I already knew that it was important to eat the right things and walk every day. Take your medications and ask questions—don’t be afraid to speak up and learn what works best for you. And lean on your family or support system. We help each other out, and that makes all the difference.”
John Smith (T2D)
Wrap Up Tips
- Address participant questions: Gather any final questions from the group and affirm the list of participants’ questions from the beginning of the session has been completed. If questions fall outside the scope of today’s lesson, invite the participant to return to future sessions to learn more about their area of interest.
- Complete Participant Journaling prompt: Using the Beyond Diagnosis Toolkit, encourage participants to write about their initial thoughts, questions, and feelings regarding their diagnosis on the final page of the Decoding Diabetes section (p. 17 in the T1D toolkit and p.16 in the T2D toolkit) in their provided toolkits. Completing the reflection is an educational tool that improves education retention among participants and personalizes the learnings to each adult.
- Develop a Personal Action Plan: Briefly demonstrate the importance of how to take action on diabetes management and diabetes knowledge goals.We have listed the prompts in the “Decoding Diabetes” section alongside reasonable action plans that participants could take to take the next step in their individual journey with diabetes. These are examples of possible actions; please take the time to help each participant create relevant action plans for their own journey!
Reflection Prompt |
Possible “Action Plans” for Participant Responses |
| Write down how you feel about having diabetes. |
|
| List three things you’d like to tell a friend, family member or partner about your diabetes. |
|
| What challenges are you facing with your diabetes? |
|
| What are your goals when it comes to living your best life with diabetes? |
|
| What healthy changes did you make today—or this week—that will lead you closer to reaching your goals? |
|
- Next Steps: Mention the next session’s topic (Creating Your Best Path Forward) and provide the date, time, and location for the next session. Encourage attendees to attend the session with a friend or support person. Remind participants to bring their BT1 or BT2 Beyond Diagnosis Toolkit with them to the next session. Encourage participants to make a list of relevant questions to bring to the next session.
- Peer support and community building: Encourage participants to share their experiences and build connections (optional)

Section 2
Creating Your Best Path Forward
Instructors can seamlessly present the lesson using the corresponding BT1 Creating Your Best Path Forward presentation (with speakers notes) and the BT1 and BT2 toolkits Creating your best path forward section (p. 19-31 for T1D Toolkit and p. 18-30 for T2D Toolkit). The participants’ toolkits include engaging visuals, diabetes ambassadors, and educational resources that correspond with your instructor slides and speaking notes. Let’s get started!
Introduction Tips:
- Welcome and program overview: Briefly introduce yourself, the program, and the learning objectives for the session.
- Encourage participants to introduce themselves: Build camaraderie within your group through introductions.
- Make a list of the group’s curiosities: Encourage each person to share one thing they hope to learn in today’s session. Record each participant’s learning objective so each item can be addressed during the education session.
- Materials distribution: Ensure all participants have a copy of the Beyond Diagnosis toolkit. Today’s session will cover reference pages 19-31 for T1D Toolkit and pages 18-30 for T2D Toolkit.
- Introduce your group to BT1 creating your best path forward T1D ambassador, Missy Leiting and T1D ambassador Keith Grear.
Education
Blood Glucose Management
Blood glucose management is the critical endpoint for evaluating successful diabetes management. For decades, research has shown strong correlations with improved blood glucose control and reduced risk of health problems from diabetes.K As diabetes care advocates, our work is not yet complete! According to the Centers for Disease Control (CDC), only 1 in 4 adults living with diabetes achieve target goals for blood glucose (hemoglobin A1c), cholesterol, and blood pressure.
As discussed in the previous module, Decoding Diabetes, there are several key self-management strategies that are shown to be effective at managing blood glucose. The ADCES7 Self-Care behaviorsM are:
- Problem Solving: Everyone encounters challenges with their diabetes management. People living with diabetes (PWD) can’t plan for every situation they may face, but there are some problem-solving skills that can help them prepare for the unexpected—and make a plan for dealing with similar problems in the future.
- Reducing Risks: By understanding the risks that cause negative outcomes and then taking actions to prevent them, PWD can lower their risks of developing diabetes-related health problems.
- Monitoring: Regularly checking blood glucose levels and other key health factors (e.g. blood pressure, kidney and foot health) gives PWD vital information to help them make decisions about diabetes.
- Taking Medication: Medications work together to lower blood glucose levels, reduce your risk of diabetes-related health problems, and help you feel better. Encourage PWD to take their diabetes medication every day for the best results.
- Healthy Eating: Having diabetes doesn’t mean PWD have to give up your favorite foods or stop eating in restaurants. Instead, encourage PWDs to focus more on knowing how foods they eat affect their blood sugar levels so they can adjust their medication. Eating nutritious foods is the goal for everyone, not just those with diabetes.
- Being Active: Movement has many health benefits that impact diabetes management like lowering cholesterol, improving blood pressure, lowering stress and anxiety, and improving mood.
- Healthy Coping: It’s natural for PWD to have mixed feelings about the challenges of diabetes management and experience highs and lows along their journey. The important thing is to recognize these emotions as normal and take steps to reduce the negative impact they can have on your self-care.
Reinforcing these key diabetes self-care behaviors will improve participants’ understanding of the strategies available to them to manage their blood glucose levels. Creating awareness around the unique biological, environmental, behavioral, pharmaceutical, nutritional, and activity-based factors that can be at play gives healthcare professionals and PWD alike an appreciation for how complex managing blood glucose can be.
Where To Start
Common Blood Sugar Goals (for Adults)
The American Diabetes Association recommends PWD achieve a hemoglobin A1c target of less than 7% for most adults*. This is based on important research demonstrating that keeping blood sugars in this healthy range will protect against health problems caused by diabetes.K Staying as close to an A1C in this healthy range will protect your body from many of the health problems that prolonged high blood sugars from diabetes can cause.
A1c Targets for Adults with Diabetes |
|
|---|---|
| American Diabetes Association | <7% |
| American Association of Clinical Endocrinologists | <6.5% |
*Each individual should work with their health care team to personalize these glucose goals for their health goals. For elderly individuals, these glucose goals may be relaxed to prevent unnecessary low blood sugar. For adults planning or experiencing pregnancy, these glucose goals are much tighter to protect the growing baby from elevated blood glucose which can interfere with the baby’s growth and development.
Remember, only 1 in 4 PWD achieve their A1c goal.L Achieving an A1c of less than 7% can be challenging; it’s common for PWDs to be unsure of what steps to take to bring the A1c level down into the healthy range. Breaking this A1c goal into smaller steps in order to achieve it can create a roadmap for how to get there. By aiming for pre-meal glucose ranges of 80-130 mg/dL and post-meal (2 hours after eating) blood glucose of less than 180 mg/dL, an A1c of less than 7% is possible. If PWDs are not seeing glucose values in these ranges, it is a sign that parts of their diabetes care plan need adjusting– for example, medications, nutrition, or activity. Checking glucose daily is an important skill to reinforce because obtaining these glucose values assists with problem solving and creating an action plan when blood glucose targets are out of range.
Common Blood Glucose Goals for Adults with Diabetes |
|
|---|---|
| Fasting, pre-meal, bedtime, overnight | 80-130 mg/dL |
| Post meal (2 hours after eating) | Less than 180 mg/dL |
Additionally, the chart below shows an average blood sugar and how it corresponds to an A1c test. This chart shows us that an A1c of 8.5% means that the average blood sugar for a person with an A1c in this range would have an average blood glucose of 197 mg/dL. In order to achieve an A1c in the target range, this individual can begin by investigating their fasting and post-meal blood glucose values to determine how they correspond to the goals (80-130 mg/dL and less than 180 mg/dL, respectively). It is likely that blood glucose checks will capture areas for when glucose values can be optimized with medication and/or lifestyle improvements. Further, this chart demonstrates the progressive nature of changes to glucose and how they translate to an A1c. Ideally, reducing the A1C to achieve the healthy range of less than 7% is the goal for all PWD, though any progress towards these targets is beneficial, protective to the health of the PWD, and should be encouraged/celebrated.
Conversion of Average Blood Glucose (mg/dL) to A1C |
|
|---|---|
| 126 mg/dL | 6% |
| 140 mg/dL | 6.5% |
| 154 mg/dL | 7% |
| 169 mg/dL | 7.5% |
| 183 mg/dL | 8% |
| 197 mg/dL | 8.5% |
| 212 mg/dL | 9% |
| 226 mg/dL | 9.5% |
| 240 mg/dL | 10% |
| 255 mg/dL | 10.5% |
Utilizing a continuous glucose monitor (CGM) is a useful tool to provide real-time feedback to the PWD regarding their blood glucose and deliver nuanced insights regarding overall blood glucose patterns/trends. CGM is particularly useful for those using insulin, and is becoming a standard of care for those with T1D. Use of CGM for those with T2D is also increasing in popularity. For the PWD, the difference between traditional blood glucose monitoring and CGM is easily compared by considering the differences between taking a photograph (traditional blood glucose reading) as compared to watching a movie (CGM readings and trends throughout the day). Both are valuable and provide insights to the PWD, but they are not the same (in ways that can be understood by comparing the difference between looking at a photograph vs watching a movie).
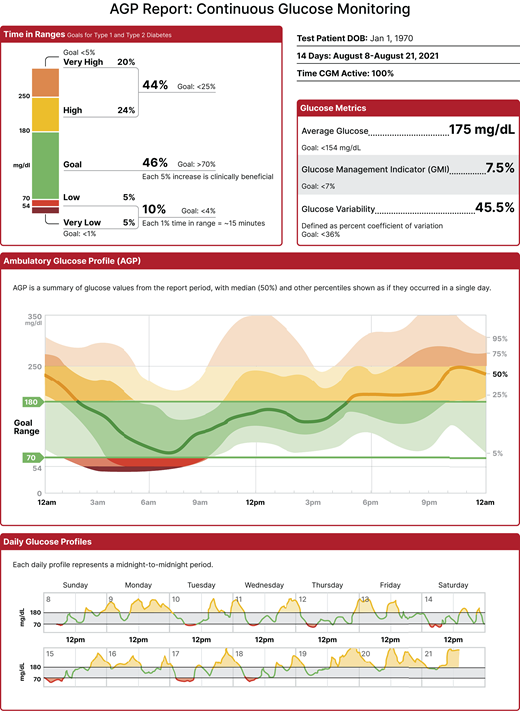
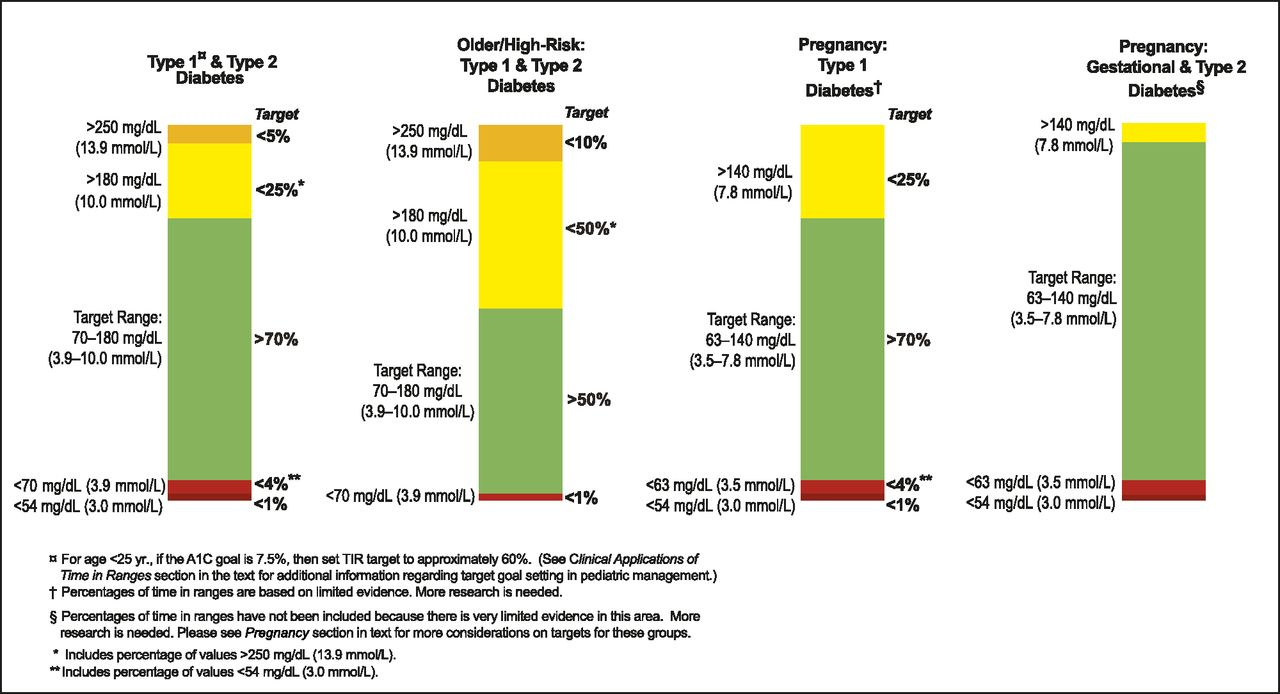
To the left is a sample CGM report B (called “ambulatory glucose profile) which provides complete statistics for an individual using CGM. Aiming for a glucose range of 80-180 mg/dL and staying in this range for 75% or three-quarters of the time. This target range for CGM is customized to each person’s unique goals (see table above) Common CGM targets are:
- At least 70% of the day in 70-180 mg/dl (in-range)
- Less than 4% of the day below 70 mg/dl (below-range)
- Minimize time each day above 180 mg/dl (above-range)
Blood Glucose Management
Quiz Time
Instructors should read the quiz questions aloud to the group. Provide 15-30 seconds of quiet time for the participants to answer the questions individually or as a group. The instructor can answer the Creating Your Best Path Forward Quiz Time questions (slide 8) using the responses and rationales provided in the table below:
Question |
Correct Answer |
Rationale |
| What is a healthy hemoglobin A1c level? | Less than 7% | Research has shown keeping the A1c below this level is a healthy range and will prevent health problems from prolonged high blood sugar. |
| What’s a common blood sugar target before meals? 80-130 mg/DL or less than 180? | 80-130 mg/dL. | Blood sugars should be at the lower range of 80-130 mg/dL before meals. Food usually increases our blood glucose, so we want to start meals at a lower number. |
| What is a good target for a blood sugar reading that’s taken after a meal (2 hours after eating)? | less than 180 mg/dL | Blood sugars are impacted by food. Blood glucose rises when we eat. Staying below 180 mg/dL allows us to enjoy a variety of nourishing foods while also keeping our body safe from prolonged high blood sugars. |
| For people using CGM, how much time do we want to spend in our target range of 80-180 mg/dL? 50%? 70% 100%? | We should aim for 70% of the time to be spent in the healthy blood sugar range (80-180 mg/dL) | Staying in the target range as much as possible is important to protect our health and body. We want to have the best blood sugar readings we can reasonably achieve. Because diabetes means that we experience higher than normal blood sugars, it is often not feasible to spend 100% of time in the target range without undue stress and restriction on someone’s life. Aiming for spending 70% of time in range is a better goal as it is enough to protect our bodies from the harm of prolonged high blood sugar but it also allows for natural blood sugar fluctuations after meals (which are common even in people who do not live with diabetes). |
Encouraging participants to be curious about their glucose values and promoting critical thinking to develop problem-solving skills is highly recommended. The PWD is a key stakeholder in the management of diabetes, and without his or her participation the healthcare team may not be alerted to make necessary changes to an individual’s diabetes regimen.
A blood glucose problem-solving framework can be found in the toolkits (page 23 of T1D toolkit and page 22 of the T2D toolkit) and on slide 9 in the Module 2 presentation (Creating Your Best Path Forward). The framework emphasizes the importance of determining a glucose goal that’s right for the PWD, keeping track of one’s blood glucose values, troubleshooting when glucose values are not within this goal range, and working with the health care team to improve blood glucose results.

- STEP 1 is to work with your healthcare team to customize these glucose target goals for your specific situation.
- STEP 2: Then, use a meter or CGM to keep track of your levels. The PWD will become familiar with their glucose results and patterns by doing this and can alert healthcare professionals when critical changes occur.
- STEP 3: The PWD can review their blood sugar patterns, play detective to determine the cause of out-of-range values and develop a plan for what comes next. They can ask why did this happen? What could have caused this out-of-range number? If the PWD notices blood sugar changes that are unexplained, encourage them to play detective and try to determine the cause. Some of the factors that can influence blood glucose can offer helpful clues.
- STEP 4: The PWD can work with their healthcare team to improve blood glucose results. The PWD may need to adjust their medication dose or try new lifestyle behaviors to make improvements. Aiming to keep blood glucose in the healthy range is important for their long-term health. If the PWD is not sure what to do to improve blood glucose results, work with a diabetes care and education specialist.
Individual Reflection: Instructors should allow participants an opportunity to try this blood glucose problem-solving framework to consider a glucose value from their journey. Encourage participants to work together to consider variables and causes to glucose results. Foster an attitude of positive curiosity that results in taking action.
Hypoglycemia
Low blood sugar, also called hypoglycemia, is when your blood sugar level drops below 70 mg/dL. Low blood sugar is URGENT and needs attention.
- Mild low blood sugar: Or a blood sugar of below 70 mg/dL. Symptoms include feeling hungry, nervousness, shakiness, cold/clammy skin, headache, pounding heartbeat, shaking, or jitters. The most common treatment is to consume fast-acting carbohydrate through foods or drinks like glucose tablets, a small glass or fruit juice, one 4 ounce juice box, or a tablespoon of honey. The PWD can repeat this step if the blood sugar does not rise (back into the healthy range) within 15 minutes. Usually mild low blood sugars are easily treatable yourself and require assistance from others.
- Moderate low blood sugar or a blood sugar of below 54 mg/dL This blood sugar is lower than a mild low blood sugar but not as low as a severe low blood sugar. The PWD may experience symptoms of dizziness, sleepiness, weakness, irritability, trouble speaking, or confusion. The best treatment for a moderate low is the same as for a mild low blood sugar. check your blood sugar then consume fast-acting carbohydrate through foods or drinks like glucose tablets, glucose gel, a small glass or fruit juice, one 4 ounce juice box, or a tablespoon of honey. The PWD can repeat this if the blood sugar does not rise within 15 minutes. Most moderate low blood sugars can be easily treatable yourself and most of the time do not require assistance from others or healthcare professionals.
- Severe low blood sugar is a blood sugar reading of less than 54 and/or with symptoms such as loss of consciousness, seizures or convulsions, or even a state of coma. Severe low blood sugars often require assistance from others to treat. Because the person experiencing a severe low blood sugar may not be conscious, the best treatment for a severe low blood sugar is GLUCAGON. Glucagon is a hormone that your body produces to INCREASE blood sugar. This is the OPPOSITE of insulin, which DECREASES blood sugar. Family, friends, paramedics, and medical staff administer glucagon to quickly raise someone’s blood sugar without the need to consume food. Glucagon is available in a nasal spray, auto-injector pens, prefilled syringe pens, or a powder that must be mixed with a liquid and drawn into a syringe before injecting. If the person is still conscious, consuming fast-acting carbohydrate will work too. Don’t wait for a severe low blood sugar to get better on its own, it’s an emergency!
Tip: Once your doctor gives you a prescription for glucagon, pick the medication up at your local pharmacy and keep it in a place that others know about. If you take insulin to treat your diabetes, the PWD should also have glucagon on hand as a safety precaution. Make sure your friends, family, roommates, and/or coworkers know that you have diabetes, know where your emergency glucagon is located, and have been trained on how to use it. You want others to know how to use glucagon in case there is an emergency situation where you need help and can’t treat your own low blood sugar without their help. Being prepared before this happens will help everyone know what to do if something like this happens and feel ready to help immediately if it does happen.
Here are some training videos to get you started.
- How to use a glucagon emergency kit: https://www.youtube.com/watch?v=ZUlx6F63gj0
- How to use a glucagon injector pen: https://www.youtube.com/watch?v=9RxvgQjFwl4&t=2s
- How to use baqsimi: https://www.youtube.com/watch?v=iReyEfsetWQ
What foods are best to treat low blood sugar?
To start, treat hypoglycemia with 15 grams* of simple carbohydrates from:
- Glucose tabs (4 tablets)
- Glucose gel (1 tube)
- Regular soda (4 ounces or half cup)
- Juice (4 ounces or half cup)
- Granulated sugar (4 teaspoons)
*The number of carbs to treat a low should be personalized
A simple place to start is to consume 15 grams from one of the sources above. Typically, within 15 minutes, blood sugar will have raised and symptoms should improve, too. However, the amount of fast acting carbohydrate each individual needs may vary (and can vary for each low blood sugar event). It can be common that when you experience a low blood sugar, the PWD may want to consume MORE than this amount of food. Stick to this amount. Eating too much of a fast-acting carbohydrate food isn’t the best idea as it can lead to a high blood sugar.
Hypoglycemia
Quiz Time
Instructor to ask group participants answers to the following questions. Use the rationale provided to answer additional questions.
- What number indicates a low blood sugar?
- less than 70 mg/dL
- What is the best way to treat a mild or moderate low blood sugar?
- The most common treatment is to check your blood sugar then consume fast-acting carbohydrate through foods or drinks like glucose tablets, a small glass or fruit juice, one 4 ounce juice box, or a tablespoon of honey. You can repeat this if the blood sugar does not rise within 15 minutes. Usually mild low blood sugars are easily treatable yourself and don’t require help from other
- Which should you use to treat a SEVERE low blood sugar of less than 54 mg/dL and have lost the ability to swallow? Glucagon or Insulin?
- GLUCAGON raises blood sugar. Insulin decreases blood sugar and will make a severe blood sugar WORSE. Do not give insulin to someone with a severely low blood sugar. Your friends and family should know where your glucagon is located and how to administer it in the event of an emergency.
- What are the types of glucagon that are available?
- Glucagon is available in a nasal spray, Autoinjector pen, Prefilled syringe, or a powder (must be mixed with a liquid before injecting)
Hyperglycemia
High blood glucose levels are above 180 mg/d and are considered dangerously high when they are over 300 mg/dL. Glucose that stays elevated for prolonged periods of time can lead to microvascular and macrovascular complications. Regularly checking blood glucose and maintaining self-care behaviors for diabetes management are paramount to optimal blood glucose control. Identification of high blood sugar (fasting, A1c, glucose tolerance test) are diagnostic indicators to confirm presence of diabetes, and continued monitoring of these parameters assure optimal health for the PWD.
Some causes of high blood sugar can include:
- Taking too little insulin or not using enough diabetes medication
- Under-counting carbohydrates at mealtimes
- Stress
- Not exercising as much as planned
- Fluctuating hormones
- Being sick or fighting an infection—including recovering from an injury or recent surgery
- Emotional stress
- When insulin has expired—or if it doesn’t work as well because it was exposed to extreme heat or cold
High blood sugars can cause specific symptoms in PWD. They are:
- Unquenchable thirst
- Dry mouth
- Feeling tired or fatigued
- Frequent trips to the bathroom to urinate
- Blurry vision
- Frequent infections
- Slow healing cuts or sores on your skin
*Symptoms tend to be more severe when blood glucose has been elevated for prolonged periods of time. When changes to blood glucose are progressive and subtle over time (mostly T2D), many of these symptoms may not be immediately obvious to the individual with elevated glucose.
Identifying hyperglycemia requires ongoing blood glucose monitoring. PWD may not experience noticeable symptoms when they experience hyperglycemia and therefore may not be prompted to take action (other than by glucose readings that are elevated). Identifying the root cause of the hyperglycemia may not always be possible, but an effort to solve the problem will likely assist the PWD in determining the next steps in their action plan for managing the hyperglycemia.
How should a PWD treat high blood sugar?
- Adjust medications/insulin doses based on instructions from their doctor or diabetes specialist
- Drink water or sugar-free electrolyte solution to help their kidneys remove sugar through urine
- If blood glucose is abnormally high (above 250mg/dl for 3 or more hours), contact your healthcare team
- If you’re vomiting and can’t keep fluid down, go to the emergency department
- If you’re sick, follow sick-day rules. Blood sugar tends to run higher during illness and stress and require an increase in diabetes medication while the PWD is experiencing (temporary) illness.
- Verify the expiration date on the diabetes medication to make sure your medications/insulin hasn’t expired. Also check that the medication has not been exposed to heat or cold, or otherwise deteriorated in quality.
- Take note of any reasons or potential changes to your routine that may be contributing to high blood sugar:
- What did the PWD eat or drink?
- Did the PWD eat something higher in carbohydrates than usual?
- Is the PWD experiencing more stress than usual?
- Is the PWD getting enough sleep?
- Is the PWD traveling or has their exercise/eating schedule changed significantly?
Remember: encourage participants to ACT on elevated blood sugar readings. It is essential that PWDs do not delay or “wait to see if it gets better” without taking action to bring the glucose back into the healthy range. Once the high glucose is identified, they should create a plan and get started to get that blood sugar back down into the healthy range quickly.
Solving for elevated blood glucose readings first thing in the morning can be a common challenge. Food is less likely to be the culprit of glucose elevations at this time of day.
The American Diabetes Association suggests the following as PWD identify the culprits of high blood glucose during the morning:
If the data shows you’re high at bedtime, the culprits are likely food and medication.
- If you have high blood glucose before you go to sleep, the elevated level can persist until morning. A large dinner or a snack at bedtime can cause elevated blood glucose levels that last all night, as can too low a dose of insulin with your evening meal. Adjusting your medication or what and when you eat may help.
If the data shows you’re in range at bedtime, the culprit is likely too little medication.
- You may go to bed with blood glucose levels within your target range, but that doesn’t mean they’ll stay that way overnight. For example, if you are taking a long-acting insulin in the morning and it wears off before the next dose the following day, you would see morning high blood glucose. Changing the timing of your long-acting insulin injection, or switching to a twice-daily basal insulin or an ultra-long-acting insulin, might fix the problem.
If the data shows you’re high in the wee hours, the culprit is likely dawn phenomenon.
- If you’re experiencing the dawn phenomenon, which raises your blood glucose between approximately 3 and 8 a.m., your doctor may recommend that you avoid increasing your long-acting insulin. While a higher dose of insulin will bring your morning highs down to normal, it could cause too great a drop in your blood glucose after you first go to sleep, but before your blood glucose starts to rise in the early hours of the morning. Sometimes the only way to adequately address the dawn phenomenon is with an insulin pump, which you can program to automatically deliver more insulin in the early morning hours.
If you don’t use insulin, it may take a good bit of trial and error before you and your health care provider figure out the best medication and lifestyle strategy to help reduce morning highs.”
Diabetic Ketoacidosis (DKA): A Special consideration for those with T1D
If any members of your group have T1D, please be sure to provide this additional life-saving information about DKA. Those with T1D can experience DKA, but it is rare in T2D.
In those who take insulin or have T1D, acting on high glucose readings is critical and can be life saving. High blood sugar can accelerate and become more serious when it turns into DKA. Many people with T1D may have experienced DKA when they were first diagnosed with diabetes. The goal is to prevent high blood sugar from turning into DKA, and this can be done by regularly checking your blood sugar and acting on elevated blood sugar levels to STOP DKA from happening.
What is DKA?
“When the body’s cells don’t get the glucose they need for energy, the body begins to burn fat for energy, which produces ketones. Ketones are chemicals that the body creates when it breaks down fat to use for energy. The body does this when it doesn’t have enough insulin to use glucose, the body’s normal source of energy. When ketones build up in the blood, they make blood more acidic. Because the human body is highly sensitive to acid/base balance or pH balance, this change in acidity can cause problems quickly. The presence of ketones are a warning sign that blood sugar is dangerously high. High levels of ketones can poison the body and cause damage. When glucose and ketone levels get too high simultaneously, you can develop DKA. DKA may happen to anyone with diabetes, though it is rare in people with type 2. DKA is an emergency and means that the body needs insulin and medical attention ASAP. Treatment for DKA usually takes place in the hospital.” PWT1D can help prevent DKA by learning the warning signs and checking your urine and blood regularly, acting to treat high blood sugars before they become an emergency.
How can I check for ketones? It is recommended that PWD check for ketones when blood glucose is greater than 250 mg/dL. This can be done by checking urine ketones or through a meter that measures ketones in your blood. Urine ketone strips are affordable and available at a local pharmacy (no prescription needed). A blood ketone meter is a medical device requiring a prescription that your doctor will prescribe. It functions similar to a blood glucose meter, except that instead of measuring glucose, it measures ketones. Contact your healthcare provider if you check your ketones with urine strips or with a ketone meter and find that ketones, especially moderate or large ones, are present in your body.
What are the warning signs of DKA? DKA usually develops slowly. But when vomiting occurs, this life-threatening condition can develop in a few hours. Early symptoms include the following:
- High blood glucose AND moderate or large urine/blood ketones
- Nausea
- Vomiting
- Abdominal pain
- Fruity or acetone breath (similar to the scent of nail polish remover)
- Rapid breathing
- Flushed Skin
- Lack of energy
As DKA worsens, other severe symptoms can appear:
- Constantly feeling tired
- Dry or flushed skin
- Nausea, vomiting, or abdominal pain. Vomiting can be caused by many illnesses, not just ketoacidosis. If vomiting continues for more than two hours, contact your healthcare provider.
- Difficulty breathing
- Fruity odor on breath
- A hard time paying attention, or confusion
Again, our best defense against high blood sugar and DKA is regular blood glucose checks. By keeping a close eye on what’s happening with your glucose, you have the necessary information to make treatment decisions and bring blood sugars back into the healthy range. If blood sugar is elevated, ACT and don’t delay!
Diabetes Technology
Below are descriptions, images, and links of available diabetes technologies in 2025.
Glucose Monitoring Technologies
Glucose Meters
A glucose meter—also called a “glucometer”—is a medical device for determining the approximate glucose concentration in blood. The user inserts a glucose “test strip” into the meter, pokes their finger with a sterile lancet/lancing device, and applies the blood to the reagent strip. The glucometer measures the amount of glucose in the blood sample and records this data in the meter’s history. Glucometers are widely used to measure blood glucose and are commonly covered by health insurance plans.
Continuous Glucose Monitor (CGM)
Abbott Freestyle Libre, Dexcom G6 or G7, Medtronic Simplera
A CGM is a small, wearable device that continuously tracks your blood sugar levels throughout the day and night. These devices have alarms and alerts for glucose values that are above and below the user’s target range. Most disposable CGM sensors are inserted by the PWD at home and worn for 10-14 days.
Flash Glucose Monitor (FGM)
Abbott Freestyle Libre
This glucose sensor is similar to the disposable CGM above, except that the user must “scan” their FGM receiver or smartphone over the sensor in order to receive a glucose reading. FGM does not transmit this information to the PWD automatically. This technology offers more intermittent glucose information and requires the user to “scan” their receiver when they want to view the glucose value. This system can be lower in cost than CGM, but does not include the alarms and alerts that CGM does.
Implantable CGM
Eversense 365
This type of CGM is implanted once per year in your arm by a healthcare professional. The glucose sensor implant remains in your arm for 365 days, and the user wears a rechargeable receiver on top of it which transmits glucose readings to a smartphone.
Insulin delivery technologies
Insulin Pens
An insulin pen is a device for giving insulin injections. Insulin pens can make taking insulin more convenient because they combine the medication and syringe in one handy unit.
Inhaled Insulin
Insulin powder that is inhaled via disposable cartridges in a respiratory inhaler.
Smart Insulin Pens
Bigfoot Unity, InPen
A smart pen is a special insulin pen that works with a phone app to keep track of when and how much insulin you take. Smart pens can be reusable or they can be attachments that go on top of disposable insulin pens.
Insulin Pumps
Medtronic 770G, Medtronic 630G, Omnipod DASH
Insulin pumps are small, computerized devices. They are about the size of a pager and deliver insulin doses on a pre-programmed schedule. These devices require the user to input all necessary information (ie, carbohydrates, blood glucose, and activity) into the pump to administer or change the insulin dosing program. Traditional insulin pumps operate as a standalone delivery system which require a blood glucose meter and/or CGM to provide necessary glucose information.
Non-Programmable Disposable Patch Pumps
CEQUR Simplicity, VGO
These are wearable insulin delivery devices designed for convenience and ease of use. They provide continuous insulin infusion without the need for complex programming.
Closed-Loop Insulin-Delivery Systems
Omnipod 5, Tandem Control IQ, Tandem Mobi, Medtronic 780G, Sequel Twiist, Beta Bionics iLet, OpenAPS*, Loop*
Some people with T1D use an insulin pump and real-time continuous glucose monitor (CGM) that “talk to each other.” This is possible through a computer program on your phone or inside the pump. Closed-loop insulin-delivery systems work to mimic the human pancreas by using CGM data to determine when it should or shouldn’t make adjustments to the wearer’s insulin delivery. Closed-loop systems have been around since the early 2000s, but they’ve seen their greatest strides in the past few years.
*not FDA approved
Wrap Up Tips
- Address participant questions: Gather any final questions from the group and affirm the list of participants’ questions from the beginning of the session has been completed. If questions fall outside the scope of today’s lesson, invite the participant to return to future sessions to learn more about their area of interest.
- Journaling prompt: Guide participants to write about their initial thoughts, questions, and feelings regarding their diagnosis in their provided toolkits. The Creating your best path forward journaling prompts can be found on pages 19-31 for T1D Toolkit and pages 18-30 for T2D Toolkit. Participants will be asked to reflect on any fears they have around living with diabetes. The reflection activity will assist participants in identifying their fears, helping them pull from prior experiences that they have overcome fear, and creating a support network and plan for how to tackle fears related to managing their diabetes.
- Medical Check-Up To Do List: Briefly discuss the importance of action planning and guide participants through using the Medical To-Do List checklist. Using the checklist will empower participants to actively monitor many of the important details of their diabetes including blood glucose, A1c, blood pressure, cholesterol, and more. . Demonstrating the importance of how to take action on diabetes management and diabetes knowledge goals models optimal self-care for diabetes and provides participants with a practical framework to use.We have listed the prompts in the “Decoding Diabetes” section alongside reasonable action plans that participants could take to take the next step in their individual journey with diabetes.
- Next Steps: Mention the next session’s topic (Fuel Well to Feel Well & Move Your Body) and provide the date, time, and location for the next session. Encourage attendees to attend the session with a friend or support person. Remind participants to bring their BT1 or BT2 Beyond Diagnosis Toolkit with them to the next session. Encourage participants to make a list of relevant questions to bring to the next session.
- Peer support and community building: Encourage participants to share their experiences and build connections (optional)

Section 3
Fuel Well to Feel Well and Move Your Body
Instructors can seamlessly present the lesson using the corresponding BT1 Fuel well to feel well and move your body presentation (with speakers notes) and the BT1 and BT2 toolkits Fuel well to feel well and move your body section (p. 32-41 for T1D Toolkit and p. 31-40 for T2D toolkit). The participants’ toolkits include engaging visuals, diabetes ambassadors, and educational resources that correspond with your instructor slides and speaking notes. Let’s get started!
Introduction Tips
- Welcome and program overview: Briefly introduce yourself, the program, and the learning objectives for the session.
- Encourage participants to introduce themselves: Build camaraderie within your group through introductions (new participants) and re-introductions (prior participants).
- Make a list of the group’s curiosities: Encourage each person to share one thing they hope to learn in today’s session. Record each participant’s learning objective so each item can be addressed during the education session.
- Materials distribution: Ensure all participants have a copy of the Beyond Diagnosis toolkit. Today’s session will cover reference pages 32-41 for T1D Toolkit and pages 31-40 for T2D toolkit.
- Introduce your group to the Beyond Diagnosis ambassadors from Fuel Well to Feel Well and Move Your Body.
Use the prompts and information provided below to lead your participants through each topic.
NOTE: If participants’ questions are detailed and require the expertise of a specialized professional in fitness or nutrition, please direct the participant or the participant’s question to the appropriate and qualified professional.
Education
Physical Activity with Diabetes
Physical activity is good for all adults*. Staying active protects the body’s bones and keeps muscles strong. According to the Physical Activity Guidelines for AmericansS, Regular movement is also one of the best ways to improve blood sugar, boost heart health, improve mood, reduce stress, and improve sleep. Just 30 minutes per day of moderate-intensity physical activity can have a big impact on blood sugar and overall health.Despite this the Physical Activity Guidelines for Americans found that “only 26 percent of men, 19 percent of women, and 20 percent of adolescents” achieve the recommended amount of aerobic and muscle-strengthening activity. The American Diabetes Association affirms these recommended amounts of physical activity for adults with T1D and T2D is the same as healthy adults. Further, research from the American Diabetes Association showed that 44.2%, 42.6%, and 65.1% of White, African American, and Hispanic individuals, respectively, met the recommended physical activity threshold.
Physical Activity Guidelines for Americans, 2020
Key Guidelines for Adults
- Adults should move more and sit less throughout the day. Some physical activity is better than none.
- Adults who sit less and do any amount of moderate-to-vigorous physical activity gain some health benefits.
- For substantial health benefits, adults should do at least 150 minutes (2 hours and 30 minutes) to 300 minutes (5 hours) a week of moderate-intensity, or 75 minutes (1 hour and 15 minutes) to 150 minutes (2 hours and 30 minutes) a week of vigorous-intensity aerobic physical activity, or an equivalent combination of moderate- and vigorous-intensity aerobic activity. Preferably, aerobic activity should be spread throughout the week.
- Additional health benefits are gained by engaging in physical activity beyond the equivalent of 300 minutes (5 hours) of moderate-intensity physical activity a week.
- Adults should also do muscle-strengthening activities of moderate or greater intensity and that involve all major muscle groups on 2 or more days a week, as these activities provide additional health benefits.
Key Guidelines for Older Adults
The key guidelines for adults also apply to older adults. In addition, the following key guidelines are just for older adults:
- As part of their weekly physical activity, older adults should do multicomponent physical activity that includes balance training as well as aerobic and muscle-strengthening activities.
- Older adults should determine their level of effort for physical activity relative to their level of fitness.
- Older adults with chronic conditions should understand whether and how their conditions affect their ability to do regular physical activity safely.
- When older adults cannot do 150 minutes of moderate-intensity aerobic activity a week because of chronic conditions, they should be as physically active as their abilities and conditions allow.
*Exercise can present specific challenges to those with retinopathy, peripheral neuropathy, or autonomic neuropathy. In some instances, these individuals with T1D and T2D should avoid exercise to prevent additional harm. If participants in the group experience any of the conditions below, encourage them to consult with their healthcare team before initiating physical activity.
- “When proliferative diabetic retinopathy or severe nonproliferative diabetic retinopathy are present, vigorous-intensity aerobic or resistance exercise may be contraindicated because of the risk of triggering vitreous hemorrhage or retinal detachment.” These individuals should work closely with their opthamologist prior to exercising.
- “Decreased pain sensation and a higher pain threshold in the extremities can result in an increased risk of skin breakdown, infection, and Charcot joint destruction with some forms of exercise. Therefore, a thorough assessment should be done to ensure that neuropathy does not alter kinesthetic or proprioceptive sensation during physical activity, particularly in those with more severe neuropathy. Moderate-intensity walking may not lead to an increased risk of foot ulcers or ulceration in those with peripheral neuropathy who use proper footwearT. In addition, 150 min/week of moderate exercise improved outcomes in people with prediabetic neuropathy. All individuals with peripheral neuropathy should wear proper footwear and examine their feet daily to detect lesions early. Anyone with a foot injury or open sore should be restricted to non–weight-bearing activities.” Low impact activities such as swimming, cycling, yoga, or pilates may be worth considering, but consult a doctor first.
- “Autonomic neuropathy can increase the risk of exercise-induced injury or adverse events through decreased cardiac responsiveness to exercise, postural hypotension, impaired thermoregulation, impaired night vision due to impaired pupillary reaction, and greater susceptibility to hypoglycemia. Cardiovascular autonomic neuropathy is also an independent risk factor for cardiovascular death and silent myocardial ischemia. Therefore, individuals with diabetic autonomic neuropathy should undergo cardiac investigation before beginning physical activity more intense than that to which they are accustomed.”
- “Physical activity can acutely increase urinary albumin excretion. However, there is no evidence that vigorous-intensity exercise accelerates the rate of progression of CKD, and there appears to be no need for specific exercise restrictions for people with CKD in general.”
There are a variety of ways to be active. Many have the misconception that physical activity can only be done at a gym or exercise center. There are a variety of daily, convenient ways to be active every day which are available to everyone. Encourage participants to select activities that are convenient and enjoyable. Any movement counts! Any progress towards the recommended amount of physical activity each day matters and improves health!
- Aerobic activity gets the heart pumping! Examples are: walking, gardening, bicycling, water aerobics, swimming, dancing, sports (tennis, soccer, basketball, hockey). Pushing a grocery cart around a store or parking your vehicle in a spot farther away from a store entrance are also daily examples of aerobic activity.
- Muscle-strengthening activities focus on using resistance to strengthen specific muscle groups. Common muscle-strengthening activities are pushups and situps, lifting weights, climbing stairs, and digging in the garden. These activities all improve the strength, power, and endurance of muscles.
- Bone-strengthening activities use movement to strengthen specific bones in your body. Some examples are running, walking, jumping rope, and lifting weights to help make bones strong for a lifetime.
- Balance activities involve the coordination of multiple limbs or muscle groups. Some examples of balance activities are walking backward, standing on one leg, walking heel-to-toe, practicing standing from a sitting position or using a wobble board to improve the body’s ability to resist forces that can make you fall.
- Flexibility activities like stretching, touching your toes, doing side stretches, and doing yoga exercises improve your flexibility and your ability to fully move your joints.
Achieving a healthy lifestyle and the recommended amount of physical activity is difficult for most adults. The American Diabetes Association recommends challenging frequent exercise obstacles and provides possible solutions to alleviate these concerns and inconveniences. During the Module 3 presentation, participants will be asked to consider their own obstacles to an active lifestyle as part of the Open Discussion prompt. Remember to allow the group to discuss these challenges at large – peer discussion and influence can be more impactful than facilitator expertise during this activity.
Overcoming Roadblocks and Getting Moving
I don’t have time to exercise for 30 minutes a day.
- Think about your day—do you have available time slots? Take advantage of any extra time that you may have and get moving. If you find yourself waiting for the kids to finish practice or watching their game from the sidelines, use that time to take a walk or pace while you watch.
- Do as much as you can. Every step counts. If you’re just starting out, start with 5-10 minutes a day and add more, little by little. Work up to three times a day.
- You can also try for 15-minute sessions twice a day.
- Make physical activity part of your daily routine. For example, walk or bike to work or to the store, exercise while you watch TV, take the stairs instead of the elevator or do something active with your family to spend time together.
I’ve never been active.
- Don’t discount your everyday activities. You may be more active than you think. Housekeeping or mowing the lawn counts as activity. Being active is more than just planned exercise.
- If you have never been active or have not been active for a while, it is important to start slowly. If you feel unsure about your health, check with your healthcare provider before making big changes in your exercise plan.
- Starting slowly is important and so is choosing activities that you enjoy. Over time, the activities you do will get easier. You will even find that you can increase the duration and/or intensity.
I’m too tired after work.
- Find a time when your energy is highest. You could plan to do something active before work or during the day. For example, you could try walking for 30 minutes during your lunch break a few days each week or hitting the gym early in the morning.
- Remember that increasing the amount of physical activity you do will actually increase your energy.
I don’t have the right clothes.
- Wear anything that’s comfortable as long as you have shoes that fit well and socks that don’t irritate your skin.
I’m too shy to exercise in a group.
- Choose an activity you can do on your own, such as following along with an exercise video or going for a walk.
- Remember that the everyday activities you do on your own like gardening and household chores get you moving and help burn calories
I don’t want to have sore muscles.
- Exercise shouldn’t hurt if you go slowly at first. Choose something you can do without getting sore.
- Make sure you warm up and cool down.
I’m afraid my blood glucose level will drop too low.
- The people who need to be most careful about lows are people with type 1 and those who are on insulin or medications that can cause low blood glucose. If you’re taking a medication that could cause low blood glucose, talk to your health care provider about ways to exercise safely.
- Always be prepared. Make sure you’ve got some regular soda or sports drink (not diet), glucose tabs, or another fast-acting carbohydrate to treat a low if one should occur. Wearing a diabetes ID is another important safety precaution.
Walking hurts my knees.
- Try chair exercises, swimming, biking, or an elliptical machine. These and other low-impact exercises may be less painful.
It’s too hot outside.
- If it’s too hot, too cold, or too humid, walk inside at a school gym or a shopping center.
- Think of some other activities that are always available regardless of the weather like using a stationary bike, indoor aerobics classes, yoga videos at home, indoor swimming, stair climbing, calisthenics, or dancing.
It’s not safe to walk in my neighborhood.
- Find an indoor activity, such as an exercise class at a community center.
- Think of activities you can do in the safety of your home.
I’m afraid I’ll make my condition worse.
- Remember that getting enough physical activity is important for everyone’s general health—whether you have diabetes or not.
- Remember that exercise helps lower A1C and has many other health benefits.
- If you have certain complications from diabetes and are unsure about your health, talk to your doctor before making any big changes to your fitness routine.
I can’t afford to join a fitness center or buy equipment.
- Do something that doesn’t require fancy equipment, such as chair exercises, walking or using water bottles for weights. Jumping rope and resistance band exercises are activities that only require one piece of inexpensive equipment.
- Look for inexpensive resources in your community like community education programs, park and recreation programs, walking trails, school running tracks, or worksite wellness programs. Your employer is another place to check for discounts on gym membership or reimbursement for fitness-related activities.
Exercise is boring.
- Find something you enjoy doing.
- Mix it up. Try different activities on different days, and make sure you pick an activity that you enjoy!
- Exercise with someone else to keep you company.
- If you can, try exercising while listening to music or watching television
I don’t really know how to exercise.
- Find a personal trainer, exercise physiologist or physical therapist to help you get started.
- Choose activities that require few skills, like climbing stairs, walking, or jogging.
- Take a class and develop new skills.
I don’t have the motivation to exercise.
- Invite a family member or friend to exercise with you on a regular basis. You can also join an exercise group or class in your community.
- Remember all of the benefits that come with being physically active.
- Make a plan so you decide when you will do each type of activity. Be sure to set realistic goals and make a plan so you know what you are working toward.
*Taken from American Diabetes Association Overcoming Roadblocks and Getting Moving
Though regular physical activity is beneficial for long-term blood glucose management, on an event-by-event basis, blood glucose results can vary significantly depending on the type, duration, and level of fitness of the individual performing the physical activity. The impact physical activity has on blood glucose isn’t always straightforward, which can make activity a confusing variable for those managing T1D and T2D. Different types of activity cause different effects on your blood glucose.
Activities that can increase blood sugar tend to activate our large muscle groups or our adrenaline response:
- Muscle- strengthening
- Resistance exercises
- Game-Days
Activities that can cause low blood sugar are usually aerobic activity. This is due to the activity’s main fuel source being fueled by the glucose in our blood stream. If the activity lasts long enough or is intense enough, these common heart-pumping activities can result in low blood sugar:
- Aerobic activity
- Walking, running, jogging
- Biking
- Swimming
- Dancing
- Sports
Activities that have little impact on blood sugar are lowest in intensity. These activities may also be a great starting point for beginners or those who have not been active recently. These activities are still important for those who are active as they strengthen muscles, prevent falls, and reduce muscle stiffness.
- Flexibility exercises
- Balance activities
- Stretching
Hypoglycemia
If glucose falls to 100 mg/dL or below, stop activity and treat the low blood sugar immediately. Glucose can drop rapidly during exercise, so consuming carbohydrate before a clinically low blood glucose (70 mg/dL) is necessary to stop a plummeting glucose trend before it results in clinically significant hypoglycemia. For hypoglycemia before, during, or after exercise, consume fast-acting carbohydrate immediately using the 15-15 rule
- Check your blood sugar
- If your blood sugar is less than 100 mg/dL during activity, consume 15-20 grams of fast-acting carbohydrate such as glucose tabs, glucose gel, sports drink made with sugar, or 4 oz juice.
- Wait 15 minutes for blood sugar to increase.
- Once 15 minutes has passed, re-check your blood sugar.
- If the blood sugar is less than 100 mg/dL when you re-check, repeat the rule of 15 by consuming an additional 15 grams of fast-acting carbohydrate.
- You can resume activity once your blood sugar raises to 100 mg/dL or higher.
Those with T1D or who use insulin, should work with their healthcare team to adjust their insulin dosage based on your blood sugar readings and how your body reacts to the exercise. This may require adjustments to basal insulin and/or bolus insulin. Adjusting insulin for moderate and intense physical activity can be a more practical strategy than consuming fast-acting carbohydrate to fuel the duration of physical activity.
Learning how to manage low blood sugar during exercise can be complex, but BT1 has some additional guidance to make it simpler. CONSIDER SHARING THESE RESOURCES:
- How to Prevent Lows During Exercise with Exercise Itself
- Don’t Crash: How to Manage Exercise Lows
- Blood Sugar Control—During and After Exercise
- Avoid Exercise Lows: How to Time Your Workouts Around Insulin Doses
Hyperglycemia
During muscle-strengthening activities like weight lifting or high-intensity exercise, it is more common to observe high blood sugar. These exercises stimulate large muscle groups which release energy into the bloodstream and may also trigger the adrenaline/stress response which can also increase your blood sugar. This is particularly true for athletes who participate in competitive or group sports. On game or competition days, adrenaline responses can increase blood sugar. In this event, work with your healthcare team to adjust the timing and amount of insulin doses or experiment with exercising at different times of day.
Learning how to manage high blood sugar during exercise can be complex, but BT1 has some additional guidance to make it simpler CONSIDER SHARING THESE RESOURCES:
- How to Balance Your Insulin Dose With Your Exercise
- Blood Sugar Control—During and After Exercise
- Anticipate the Rise: How to Manage Exercise-Induced Highs
Activity Tips and Hacks for Diabetes
Before Exercise
- Check blood sugar levels to avoid hypoglycemia
- Pack fast-acting sugar and diabetes medications (ie, insulin) on hand for the entire duration of your activity.
- Adjust medication doses prior to activity, as needed
During Exercise
- Monitor blood sugar changes using a blood glucose meter. Consume 15 grams of fast-acting sugar if glucose is 100 mg/dL or less at any point during activity.
CGM are helpful to track the glucose trend but the results may lag behind during rapid blood glucose changes during activity. It is best to check glucose with a meter during exercise. - Have the following on hand:
- Diabetes supplies (meter, strips, insulin, pump supplies)
- Fast-acting sugar (sports drink, glucose tablets)
- Water
- Food
After Exercise
- Monitor your body for blood sugar changes. Check your blood sugar frequently for several hours after exercise to catch any delayed changes.
- Drink plenty of water and consider having a snack that includes protein and carbohydrates to help stabilize blood sugar levels in case needed.
- Be prepared to adjust your insulin dosage based on your blood sugar readings and how your body reacts to the exercise.
In summary,
- Being active is a lifelong goal for everyone, not just those with diabetes.
- Check blood glucose levels before, during, and after exercise.
- Use trial and error to understand the body’s response to different exercises.
- Take notes to record which strategies are best to navigate blood glucose during activity.
- Modify your plan based on the activity. Not all activities have the same impact on blood glucose.
- Evaluate which strategies work best for different types of activities or glucose patterns.
- Work with a healthcare team to develop a plan that works.
Quiz Time
1. How much exercise (such as walking) should you aim for?
A. 100 minutes per week or 20 minutes per day of high intensity activity like running
B. 150 minutes per week or 30 minutes per day of moderate-intensity activity like walking
C. 300 minutes per week or 60 minutes per day of high-intensity activity like running
ANSWER: B
- 150 minutes of moderate activity such as walking is recommended per week.
- This breaks down into about 30 minutes per day.
- Strength building or muscle-strengthening activities are also recommended at least twice per week.
2. What should you do if your blood sugar is low (ie,less than 100 mg/dL) during exercise?
A. Do nothing and keep exercising until my workout is done
B. Stop my exercise by eating a snack of 15 grams of fast-acting carbohydrates (sugar), and take a break and check my blood sugar again in 15 minutes.
C. Stop exercising in the future because activity makes my blood sugar go low
D. Stop taking my diabetes medications and not tell my doctor
ANSWER: B
- If you have low blood sugar or a decreasing blood glucose trend during activity, you need to eat fast-acting carbohydrates quickly. It is important to ACT and treat the low blood sugar before it gets too low, even if that means stopping the activity before you intend to finish.
- Consume 15 grams of glucose gel, glucose tabs, 4 oz juice or 8 o z sports drink made from sugar to raise your blood sugar quickly. Stop activity until glucose is over 100 mg/dL.
- Blood sugar can drop more quickly during physical activity because your body uses glucose as fuel for your body’s increase in activity.
- Work WITH your healthcare team to develop an exercise plan for long-term health. Do not give up activity because of the fear of low blood sugar. Do not stop taking medications completely without talking with your doctor. It can take time to create the best activity plan for your preferences and blood sugar. Be patient and ask for help!
3. Once you take a break and treat your low blood sugar symptoms during activity, when you check your blood sugar again, what number indicates that you are safe to resume exercise?
A. Above 100 mg/dL
B. 200 mg/dL
C.250 mg/dL
ANSWER: A
- Once you have consumed 15 grams of carbohydrates, waiting 15 minutes for this to take effect in your system should result in an increased blood sugar. A blood sugar of 100 mg/dL or greater indicates that your blood sugar has risen sufficiently for you to resume your exercise again.
- Eating the right amount of carbohydrates (not too much) will help you boost the blood sugar without causing a “rebound” high blood sugar from eating too much.
- You do not need to wait until glucose rises to 200 mg/dL to resume activity. This could be longer than 15 minutes, further delaying your activity.
- It is not recommended to exercise if you have a blood glucose of above 250 mg/dL- this is dangerously high and should be avoided.
Food and Nutrition Basics
One of the most common questions in diabetes self-management classes is around food and what kinds of foods are best for keeping blood sugars healthy. This can vary a lot from person to person and between T1D and T2D, and has evolved significantly over the past 35 years as supported by discoveries in nutrition science. Having diabetes doesn’t require making drastic changes to the foods we eat, though a strong foundation in healthy nutrition certainly improves health outcomes in those with diabetes. Recent nutrition guidance for diabetes aligns with other high-quality nutrition evidence from the American Heart Association, Kidney Disease: Improving Global Outcomes, Academy of Nutrition and Dietetics, European Association for the Study of Diabetes, and the Dietary Guidelines for Americans.
Dietary Guidelines for Americans 2020-2025
Follow a healthy dietary pattern at every life stage
At every life stage—infancy, toddlerhood, childhood, adolescence, adulthood, pregnancy, lactation, and older adulthood—it is never too early or too late to eat healthfully.
Customize and enjoy nutrient-dense food and beverage choices to reflect personal preferences, cultural traditions, and budgetary considerations.
A healthy dietary pattern can benefit all individuals regardless of age, race, or ethnicity, or current health status. The Dietary Guidelines provides a framework intended to be customized to individual needs and preferences, as well as the foodways of the diverse cultures in the United States
Focus on meeting food group needs with nutrient-dense foods and beverages, and stay within calorie limits
An underlying premise of the Dietary Guidelines is that nutritional needs should be met primarily from foods and beverages—specifically, nutrient-dense foods and beverages. Nutrient-dense foods provide vitamins, minerals, and other health-promoting components and have no or little added sugars, saturated fat, and sodium. A healthy dietary pattern consists of nutrient-dense forms of foods and beverages across all food groups, in recommended amounts, and within calorie limits.
The core elements that make up a healthy dietary pattern include:
- Vegetables of all types—dark green; red and orange; beans, peas, and lentils; starchy; and other vegetables
- Fruits, especially whole fruit
- Grains, at least half of which are whole-grain
- Dairy, including fat-free or low-fat milk, yogurt, and cheese, and/or lactose-free versions and fortified soy beverages and yogurt as alternatives
- Protein foods, including lean meats, poultry, and eggs; seafood; beans, peas, and lentils; and nuts, seeds, and soy products
- Oils, including vegetable oils and oils in food, such as seafood and nuts
Limit foods and beverages higher in added sugars, saturated fat, and sodium, and limit alcoholic beverages
At every life stage, meeting food group recommendations—even with nutrient-dense choices—requires most of a person’s daily calorie needs and sodium limits. A healthy dietary pattern doesn’t have much room for extra added sugars, saturated fat, or sodium—or for alcoholic beverages. A small amount of added sugars, saturated fat, or sodium can be added to nutrient-dense foods and beverages to help meet food group recommendations, but foods and beverages high in these components should be limited.
Limits are:
- Added sugars—Less than 10 percent of calories per day starting at age 2.
- Avoid foods and beverages with added sugars for those younger than age 2.
- Saturated fat—Less than 10 percent of calories per day starting at age 2.
- Sodium—Less than 2,300 milligrams per day—and even less for children younger than age 14.
- Alcoholic beverages—Adults of legal drinking age can choose not to drink, or to drink in moderation by limiting intake to 2 drinks or less in a day for men and 1 drink or less in a day for women, when alcohol is consumed. Drinking less [alcohol] is better for health than drinking more [alcohol]. There are some adults who should not drink alcohol, such as women who are pregnant.
Dietary patterns should emphasize foods and beverages with nutrient density such as vitamins, minerals, and other health-promoting components which are often found in vegetables, fruits, whole grains, seafood, eggs, beans, peas, and lentils, unsalted nuts and seeds, dairy products, and lean meats and poultry.
Eating well is one of life’s greatest pleasures. Nutrition is incredibly individual and represents personal preferences, cultural traditions, budgetary considerations, socialization opportunities, and comfort. Making healthy, balanced choices are good for everyone—not just for people who have T1D or T2D. Helping individuals living with T1D and T2D understand what—and how much—to eat and how to match insulin doses to the foods consumed is a skill that takes time to learn, but is one that is essential to master. Working with a Registered Dietitian Nutritionist to create a personalized eating plan is effective in managing T1D and T2D; “medical nutrition therapy (MNT) is associated with A1C absolute decreases of 1.0–1.9% for people with T1D and 0.3–2.0% for people with T2D.”
What Is Medical Nutrition Therapy?
MNT is nutrition-based treatment provided by a registered dietitian nutritionist who completes a thorough, personalized nutrition evaluation of an individual’s food and nutrition needs. The RDN uses this information to create an individual nutrition plan that is based on personal food preferences and proven scientific research to treat and improve certain medical conditions, like T1D and T2D. The RDN assists their clients with long-term follow-up over multiple visits and assists with behavioral and lifestyle changes. MNT can be conducted in multiple settings such as hospitals, outpatient clinics, or as part of a telehealth program. Health insurance coverage for MNT varies by individual policy though has been expanded through the Affordable Care Act. Individuals with diabetes also are eligible to receive up to 2 hours of MNT per year through traditional Medicare benefits when accompanied by a confirmed diagnosis of diabetes and referral from a physician.
Who are Registered Dietitian Nutritionists?
Registered Dietitian Nutritionists (RDNs) are food and nutrition experts with a minimum of a graduate degree from an accredited dietetics program and who completed a supervised practice requirement, passed a national exam and continued professional development throughout their careers. Registered Dietitian Nutritionists are the sole food and nutrition expert qualified to provide medical nutrition therapy.
There can be a lot of stress around eating when you first learn about T1D and T2D. It takes time to learn about the impact the foods each person consumes on blood glucose and medication regimens. Encourage participants to give themselves patience and time as they learn and experiment. If participants need assistance obtaining healthy foods and beverages, please encourage them to utilize these resources below in addition to any food pantries or charitable organizations in your local community.
What Resources Can Help With Food Access and Affordability?
SNAP: SNAP provides nutrition benefits to supplement the food budget of needy families so they can purchase healthy food and move toward self-sufficiency.
WIC: WIC safeguards the health of low-income women, infants, and children up to age 5 by providing supplemental foods, nutrition education, and healthcare referrals.
Meas on Wheels: Search for senior meal delivery and nutrition programs in your local area.
Local Food Banks: Search for food pantries and meal programs in your community through Feeding America.
Senior’s Farmers Market Nutrition Program: The Senior Farmers’ Market Nutrition Program (SFMNP) is designed to provide low-income seniors with access to locally grown fruits, vegetables, honey and herbs; increase the domestic consumption of agricultural commodities through farmers’ markets, roadside stands, and community supported agriculture programs; and aid in the development of new and additional farmers’ markets, roadside stands, and community supported agriculture programs.
Commodity Supplemental Food Program: The Commodity Supplemental Food Program (CSFP) works to improve the health of low-income persons at least 60 years of age by supplementing their diets with nutritious USDA Foods.
Veteran Food Assistance Program: The Veterans Food Assistance Program (VFAP) is designed to provide a one-time grant of essential food and household support to veterans and their families, ensuring no veteran goes hungry.
National Hunger Hotline: Call the USDA National Hunger Hotline for help finding free food in your area. You can contact the hotline by calling 1-866-3-HUNGRY or by texting the word food to 914-342-7744.
Getting Started with Eating Well for T1D and T2D
Encourage participants to get started by exploring their current nutrition choices.
- Find a nutrition baseline by writing down food, snack, and drink choices and any observations on their impact on blood glucose.
- Recording this information will help diabetes care teams identify any changes needed to the treatment regimen.
- Record the timing and frequency of meals, snacks, beverages, and treats.
- Learn to read food labels and understand recommended portion sizes.
- A registered dietitian plays a pivotal role in providing personalized nutrition guidance and can help teach label reading and carbohydrate management.
- Talk with your healthcare team about your observations. Work with a Registered Dietitian Nutritionist for specialized expertise in understanding food’s role in diabetes management.
Nutrition Tips For Eating Well With Diabetes
There really isn’t one meal plan for T1D or T2D. Help participants resist the idea that there is one “Diet” to fix T1D or T2D. Instead, shift thinking to creating a healthy meal plan or healthy eating pattern that accommodates tastes, preferences, and budget.
Here are some healthy eating principles from the Dietary Guidelines for Americans that can serve as a starting point.
- Choose whole foods (fruits, vegetables, grains, protein foods, nuts/seeds, oils, and dairy) located in the perimeter of the grocery store instead of highly processed, packaged foods found in the center aisles.
- Choose brightly-colored non-starchy vegetables (See table below)
- Prioritize whole grains over refined grains at least 50% of the time. Choose the whole grain option (bread, rice, pasta) instead of the option made from enriched, white flour. Refined grains (e.g white bread, white rice, sugary cereals, and packaged crackers or snacks) don’t have as much nutrition as whole grain options (See table below)
- Reduce intake of added sugar. It is not beneficial for health.
- As often as possible, drink water. Eliminate beverages that are made with sugar like soda, juice, and sweetened coffee or tea.
What are non-starchy vegetables?
Dark-Green Vegetables
- Broccoli
- Bitter melon leaves, chrysanthemum leaves, escarole, nettles, poke greens, taro leaves, turnip greens
- Amaranth leaves, beet greens, bok choy, broccoli rabe (rapini), chard, collards (collard greens), cress, dandelion greens, kale, mustard greens, spinach, Swiss chard, watercress
- Raw leafy greens: Arugula (rocket), basil, cilantro, dark green leafy lettuce, endive, escarole, mixed greens, mesclun, romaine
Red and Orange Vegetables
- Carrots
- Pimento/Pimiento
- Pumpkin, calabaza
- Red and orange bell peppers
- Red chili peppers
- Sweet potato
- Tomatoes
- 100% vegetable juice
- Winter squash (acorn, butternut, Hubbard, kabocha)
Other Vegetables
- Asparagus
- Avocado
- Bamboo shoots
- Bean sprouts
- Cabbage, green, red, napa, savoy
- Cactus pads (nopales)
- Cauliflower
- Celery
- Cucumbers
- Green or wax beans
- Green bell peppers
- Lettuce, iceberg or head
- Mushrooms
- Okra
- Onions
- Summer squash or zucchini
Adapted from MyPlate Healthy Vegetables
What Are Whole Grains?
Bagels:
- 2″ mini bagel
Bagel or pita chips:
- ⅓ cup bagel or pita chips
Barley:
- ½ cup, cooked
Buckwheat:
- ½ cup, cooked
Biscuits:
- 1 small biscuit
Breads:
- 1 regular slice of bread
- 1 small slice of French bread
- 4 snack-size slices of rye bread
Bulgur:
- ½ cup, cooked
Challah bread:
- 1 medium or regular slice
Chapati:
- 1 small chapati or roti (6″)
- ½ large chapati or roti (8″)
Cornbread:
- 1 small piece of cornbread
Couscous:
- ½ cup, cooked
Crackers:
- 5 whole wheat crackers
- 2 rye crisp breads
- 7 square or round crackers
English muffins:
- ½ English muffin
Muffins:
- 1 small muffin
Oatmeal:
- ½ cup, cooked
- 1 packet instant
- 1 ounce (⅓ cup) dry (regular or quick)
Pancakes:
- 1 pancake (4½” diameter)
- 2 small pancakes (3″ diameter)
Pasta – spaghetti, macaroni, noodles:
- ½ cup, cooked
- 1 ounce, dry
Popcorn:
- 3 cups, popped
Quinoa:
- ½ cup, cooked
Ready-to-eat breakfast cereal:
- 1 cup, flakes or rounds
- 1¼ cup, puffed
Rice:
- ½ cup, cooked
- 1 ounce, dry
Tortillas:
- 1 small flour tortilla (6″ diameter)
- 1 corn tortilla (6″ diameter)
Adapted from MyPlate Healthy Grains
Diabetes Plate Method
The American Diabetes Association offers a stress-free way to plan your healthy meals without counting, calculating, or measuring. Just use a 9-inch plate to estimate portion sizes! Using this healthy plate method template also keeps carbohydrates consistent from meal to meal.
This eating strategy prioritizes balance and piles in nutritional goodness:
- Fill the plate with 50% non-starchy vegetables which are filled with fiber, antioxidants, and countless vitamins and minerals. There are so many non-starchy vegetables to choose from! They can be cooked, canned, raw, or frozen varieties. Vegetables are a nutritional powerhouse, which is why we want them to be the anchor of the plate. Choosing brightly colored non-starchy vegetables is ALWAYS a nutritious choice and ALWAYS a WIN! Feel good about choosing to eat more vegetables- at meals, at snacks, and at any time!
- Next, the healthy, balanced plate also contains lean protein foods which can come from either animal sources or plant sources of protein. Many people commonly think of protein foods like chicken, beef, pork, turkey, eggs, cheese, and fish. These animal proteins certainly belong here in the protein foods group because they are packed with muscle-building protein. But animal foods aren’t the only foods that contain protein! Surprisingly, there are many plant sources of protein, too, which research shows us are great for our health, the planet, and our wallet. Plant-based proteins like tofu (soya), beans and legumes, peanut butter, soybeans (edamame), nuts and seeds, are often more affordable choices when compared to their animal protein counterparts. Either way, choosing leaner protein sources from animal and plant sources is best for health. What’s the right portion size for all of these different protein foods? A good place to start is by placing the protein food as 25% or no more than one-quarter of the 9-inch plate. This is enough protein, but not too much. This amount of protein (25% of the plate) is often less than most people consume in the USA, so it’s important to take note of the right portion size for protein.
- The final quarter of the plate is reserved for carbohydrates- grains, starchy vegetables, or fruit. Carbohydrate foods break down into sugar in our blood. Simply put, eating carbohydrate foods increases blood sugar. Getting the right amount of carbohydrates to provide energy while not causing too much of a blood sugar rise is important and a balancing act. Plus, many people really enjoy carbohydrate foods like grains (bread, pasta, rice), starchy vegetables (potatoes, corn, peas), fruit, and milk! They belong on this healthy, balanced plate. Contrary to what you may have been told, they don’t need to be eliminated entirely. Instead choose the portion size of carbohydrate foods with intention where it can fit on the last 25% of the 9-inch plate. Enjoy carbohydrate foods- pastas, rice, bread, corn, green peas, potatoes, whole grain crackers, tortillas, popcorn, fruits, and many whole grain options like quinoa, brown rice, bulgur, and buckwheat). Good advice is to choose whole grain carbohydrates at least 50% of time. The whole grain options contain more fiber and nutrients, so consuming these choices more often is better for blood sugar and fiber intake.
Together, this balanced plate offers just the right amount of healthy food to nourish and provide energy.
Group Discussion
Participants will be asked to design a healthy, balanced meal using the plate method style of eating. The meal should include foods that each participant enjoys and fits into each of the recommended portion sizes: 50% plate is non-starchy vegetables, 25% plate is lean protein, and 25% plate is carbohydrates from grains, starchy vegetables, or fruit. Below, are sample meals that instructors can use as a guide to evaluate the participant sample meals:
The BT1 team has created a sample meal plan to get started with healthy nutrition basics for diabetes. Remember, there is no need for you to give up your favorite foods entirely– it may be a s simple as being intentional about choosing a healthy portion size or consuming a favorite food item at a particular time of day to improve your blood sugar results. Feel free to explore the recipes on the BT1 and BT2 websites for inspiration.
Featured BT1 Recipe Collection
Recipes on BT1 include:
- https://beyonddstaging.wpenginepowered.com/summer-berry-clafoutis/
- https://beyonddstaging.wpenginepowered.com/ropa-vieja/ —> need to look at the calories on this recipe
- https://beyonddstaging.wpenginepowered.com/tacos-al-pastor/
- https://beyonddstaging.wpenginepowered.com/couscous-salad-2/
- https://beyonddstaging.wpenginepowered.com/jell-o-with-yogurt-and-strawberries/
- https://beyonddstaging.wpenginepowered.com/chilaquiles-with-salsa-verde-and-chicken/
- https://beyonddstaging.wpenginepowered.com/chiles-en-nogada/
- https://beyonddstaging.wpenginepowered.com/low-carb-old-fashioned/
- https://beyonddstaging.wpenginepowered.com/fudgy-avocado-brownies/
- https://beyonddstaging.wpenginepowered.com/carnitas-posole/
- https://beyonddstaging.wpenginepowered.com/piles-and-piles-of-pancakes-and-a-kale-salad
- https://beyonddstaging.wpenginepowered.com/spring-moscow-mule/
- https://beyonddstaging.wpenginepowered.com/blackberry-mint-mojito-from-be-mixed/
- https://beyonddstaging.wpenginepowered.com/watermelon-margarita-from-be-mixed/
- https://beyonddstaging.wpenginepowered.com/spicy-margarita-from-be-mixed/
- https://beyonddstaging.wpenginepowered.com/avgolemono-chicken-soup-with-lemon-egg-and-cauliflower-rice/
- https://beyonddstaging.wpenginepowered.com/crustless-pumpkin-pie/
- https://beyonddstaging.wpenginepowered.com/cauliflower-mashed-potatoes/
- https://beyonddstaging.wpenginepowered.com/green-beans-with-goat-cheese-almonds/
- https://beyonddstaging.wpenginepowered.com/autumn-fruit-salad/
- https://beyonddstaging.wpenginepowered.com/cranberry-sauce/
- https://beyonddstaging.wpenginepowered.com/roasted-carrots-with-herbs/
- https://beyonddstaging.wpenginepowered.com/braised-chicken-with-mushrooms-artichokes-and-almond-olive-relish/
- https://beyonddstaging.wpenginepowered.com/salmon-braised-fennel-with-charred-orange-green-goddess-dressing/
- https://beyonddstaging.wpenginepowered.com/pumpkin-pie-smoothie/
- https://beyonddstaging.wpenginepowered.com/pbt-chocolate-pudding/
- https://beyonddstaging.wpenginepowered.com/chicken-avocado-and-tomato-salad/
- https://beyonddstaging.wpenginepowered.com/vegetarian-eggs-benedict/
- https://beyonddstaging.wpenginepowered.com/vegan-waffles/
- https://beyonddstaging.wpenginepowered.com/couscous-salad/
- https://beyonddstaging.wpenginepowered.com/roasted-pesto-marinated-shrimp-scallops/
- https://beyonddstaging.wpenginepowered.com/pasta-fazool/
- https://beyonddstaging.wpenginepowered.com/greek-antipasti/
- https://beyonddstaging.wpenginepowered.com/paleo-buffalo-chicken-meatballs-from-all-american-paleo-table/
- https://beyonddstaging.wpenginepowered.com/vegan-chocolate-chip-cookies/
- https://beyonddstaging.wpenginepowered.com/taco-waffles/
- https://beyonddstaging.wpenginepowered.com/maple-spice-mug-cake/
- https://beyonddstaging.wpenginepowered.com/mexican-chopped-salad-with-jalapeno-lime-dressing/
- https://beyonddstaging.wpenginepowered.com/huevos-rancheros/
- https://beyonddstaging.wpenginepowered.com/kale-lentil-and-eggplant-salad-with-pesto/
- https://beyonddstaging.wpenginepowered.com/roasted-maple-brussels-sprouts-with-apples-and-walnuts/
- https://beyonddstaging.wpenginepowered.com/the-ultimate-superfood-bites/
- https://beyonddstaging.wpenginepowered.com/cauliflower-beef-bowl/
- https://beyonddstaging.wpenginepowered.com/light-bright-and-crunchy-salad/
- https://beyonddstaging.wpenginepowered.com/morning-butter-biscuits-from-all-american-paleo-table/
- https://beyonddstaging.wpenginepowered.com/grapefruit-and-fennel-salad/
- https://beyonddstaging.wpenginepowered.com/fluffy-coconut-flour-blueberry-pancakes/
- https://beyonddstaging.wpenginepowered.com/strawberry-paleo-muffins/
- https://beyonddstaging.wpenginepowered.com/quinoa-granola/
- https://beyonddstaging.wpenginepowered.com/daikon-temaki-sushi-hand-rolls/
- https://beyonddstaging.wpenginepowered.com/gretchens-avocado-tuna-bowl/
- https://beyonddstaging.wpenginepowered.com/zucchini-noodles-with-creamy-avocado-basil-sauce/
- https://beyonddstaging.wpenginepowered.com/ginger-beef-soup/
- https://beyonddstaging.wpenginepowered.com/spaghetti-squash-casserole/
- https://beyonddstaging.wpenginepowered.com/welcome-to-chunky-town-chocolate-chip-cookies/
- https://beyonddstaging.wpenginepowered.com/fro-yo-raspberry-popsicles/
- https://beyonddstaging.wpenginepowered.com/peanut-butter-and-jelly-smoothie/
- https://beyonddstaging.wpenginepowered.com/turkey-paillards-with-cranberry-piccata-sauce/
- https://beyonddstaging.wpenginepowered.com/strawberry-seltzer/
Carbohydrate Counting
When you have T1D or T2D, understanding the role of carbohydrates in foods and how the body uses them for energy matters. In short, when carb foods are digested, the body breaks them down into glucose (sugar), which enters the bloodstream. Insulin (either insulin that our pancreas produces like in T2D or from external insulin injections, pump, or inhaler like in T1D) is needed to process the sugar and turn it into energy. Without insulin, the sugar remains in our bloodstream and cannot be used for energy. When carbohydrates are consumed, blood sugar naturally rises but the body produces insulin to offset this rise in blood glucose. However, too much carbohydrate and/or not enough insulin can cause too much of a glucose rise. Take note of the types and quantities of carb foods consumed and when/how much insulin is taken.
Carbs have a big impact on your blood sugar levels, and tracking carbohydrate intake has become an important strategy for managing blood glucose and identifying patterns in glucose variation. For those using insulin as part of their diabetes treatment plan, finding the right balance between the amount of insulin and the carbohydrate consumed will help balance blood sugar, avoiding steep highs and lows. The plate method is still a great tool for balancing the food groups of a meal to give you enough essential nutrition from each food group without causing too much of a blood sugar rise or drop. Eating carbohydrate foods alongside non-starchy vegetables and lean protein is a winning strategy for health and blood sugar regulation, too.
Keeping track of carbohydrate foods can be tiring, because carbohydrate foods are VERY common. In T1D management plans, carbohydrate estimation can be required at every meal and snack, which also adds up to a significant burden to the individual living with T1D. The use of insulin to carbohydrate ratios is common in intensive insulin management programs used in T1D and T2D management. This requires the individual with diabetes to estimate their carbohydrate intake at each meal and snack in order to determine the correct insulin dose and to respond to hyperglycemic events after eating by administering additional insulin.
The first step in learning about the impact of carbohydrate foods is by tracking it. So start with a scale and a measuring cup, and eventually look at food labels. When looking for carbohydrate values on nutrition labels, read the “total carbohydrate” line, which includes the three main types of carbs: sugars, starches, and fiber. Always check the serving size. It is common that some foods contain more than one serving per package. To determine the carbohydrate content of these items, first select the portion size that will be consumed and then multiply the total carbohydrate listed for one serving. For example: 1 cup serving = 22 grams of total carbohydrate then 2.5 cup serving = 55 grams total carbohydrate.
Because added sugar is not health promoting, we should limit it as much as possible. It’s best to avoid foods that have >20% added sugars per serving listed on the label. As you become familiar with the carbohydrate content of the foods you eat consistently, estimating the amount in your meals and snacks will become second-nature and you will find that you are more efficient in estimating the amount of carbohydrate you eat.
Many find it helpful to work with a Registered Dietitian Nutritionist as they are learning more about carbohydrate foods and the impact each of these foods has on their blood sugar. RDNs are the qualified experts to teach label reading, healthy carbohydrate choices that align with your food preferences, and create an eating plan that includes preferred foods that align with individual health and blood sugar goals. RDNs can also help explain the complex role of protein, fats, and fiber as they relate to your blood glucose readings and overall health.
For all the measuring and counting, not all foods affect all people in the same way. One great tool is to create a log or use an app to test how similar foods and portion sizes impact blood sugar, and if you take insulin, with different insulin doses. Reviewing the results several times can help you to come up with your ideal dose. With practice, you’ll become an expert at estimating portions for the foods you love. But remember, just like our ambassadors said earlier in the presentation, all of this takes time! Give yourself time to learn and explore, but reach out to helpers if you get stuck along the way.
BT1 has developed several carbohydrate counting resources to help:
- https://beyonddstaging.wpenginepowered.com/carb-count-and-t2d/
- https://beyonddstaging.wpenginepowered.com/calorie-counting-apps/
- https://beyonddstaging.wpenginepowered.com/fast-food-nutrition-guide/
Below are ideas for healthy snacks:
- Hummus with Carrots
- Celery with Peanut Butter
- Veggie chips
- Cucumber slices or cherry tomatoes
- Popcorn
- Whole wheat crackers with string cheese
- Broccoli with dip/salad dressing
- Hard-boiled egg
- Greek yogurt (no added sugar) with fruit
- Cottage cheese
- Tuna with whole wheat crackers
- Unsalted nuts (peanuts, almonds, pecans, cashews)
- Unsalted Seeds (pumpkin, sunflower)
- Clementine
- Small apple
- Tortilla chips with black bean dip or salsa
- Roasted chickpeas
Food Journaling
Encourage participants to find the food journaling pages in their BD Handbooks (page 40 for the T1D Handbook, and page 39 for the T2D handout). They can use this form as a template to create their own food journal. The journal will help each participant explore how their daily meals affect their body and blood glucose levels. Participants will be asked to estimate the total size of the meal, where the meal was consumed (at home/restaurant), the individual’s stress level when eating, how the individual felt 2 hours after eating, alongside the food and drink consumed, and their blood glucose value before eating. Most importantly, the food journal emphasizes positive learning by concluding the food logging experience with a positive reflection on what went well today so each individual can build upon their successes.
Taking Action
As with prior sections in the Beyond Diagnosis modules, helping participants wrap up their learning by planning to take action for their health is a key learning objective. Encourage each participant to set a health goal to increase their movement or eat more healthfully. Some sample actions are below:
Talk to your team
Reach out to your dietitian nutritionist or other members of your diabetes management team to discuss how to include your favorite foods into your meal plan.
Create a safe exercise plan
Collaborate with your healthcare team to develop a safe exercise plan tailored to your health status and fitness level.
Plan smart food swaps
Work with your dietitian to identify smart swaps and appropriate portions for your favorite foods. Your dietitian can help you create a meal plan that fits your preferences and nutritional needs.
Reflect on your journey
Journal and reflect on your feelings about your diagnosis and your outlook on your future with diabetes, including your relationship with food and exercise
Wrap Up Tips
- Journaling prompt: Guide participants to record their food intake for a few days using the BD FoodJournal pages in their handbook. and feelings regarding their diagnosis in their provided journals.
- Action Planning: Briefly discuss the importance of action planning and guide participants through creating one using the sample actions listed above in the Taking Action table for Section 3: Fuel Well to Feel Well and Move Your Body
- Next Steps: Mention the next session’s topic Building Your Diabetes Support Team and provide the date, time, and location for the next session. Encourage attendees to attend the session with a friend or support person. Remind participants to bring their BT1 or BT2 Beyond Diagnosis Toolkit with them to the next session. Encourage participants to make a list of relevant questions to bring to the next session.
- Peer support and community building: Encourage participants to share their experiences and build connections (optional)

Section 4
Building your Diabetes Support Team
Instructors can seamlessly present the lesson using the corresponding BT1 presentation (with speakers notes) and the BT1 and BT2 toolkits Building Your Diabetes Support Team section (p.42 for T1D Toolkit and p.41 for T2D toolkit). The participants’ toolkits include engaging visuals, diabetes ambassadors, and educational resources that correspond with your instructor slides and speaking notes. Let’s get started!
In this module, participants will be encouraged to build a support network that is meaningful, positive, and supportive to their journey with diabetes. This can take many forms- personal relationships, family relationships, healthcare encounters, peers with diabetes, or even the diabetes online community (DOC). Participants will receive an overview of which members of the healthcare team can offer support to their unique journey, learn more about the impact of diabetes on mental and emotional health, and most importantly have the opportunity to check in with their own mental and emotional health via the Emotional Check-In reflection pages in the T1D and T2D toolkits.
As instructors present this module, please be aware that there are many stigmas and misconceptions regarding both topics (diabetes and mental health). Research has shown that both diabetes and mental/emotional health carry significant stigma. There are negative attitudes, beliefs, and stereotypes about both those who live with diabetes and those who experience mental health conditions. We also know that these stigmas influence how individuals access care for both diabetes and mental health conditions. Your role as an instructor will demonstrate to the group that these misconceptions about diabetes and mental health are falsehoods. It is our goal to model that experiencing challenges along the journey of T1D and T2D is normal and that effective mental and emotional health treatment can help! Your role modeling as an instructor on this important topic will demonstrate to participants how to take care of their emotional health, build a strong and meaningful support network and to effectively navigate some of these challenges positively.
The Behavioral Diabetes Institute provides Diabetes Etiquette tips for those without diabetes to provide better support to those who live with T1D or T2D.
- DON’T offer unsolicited advice about my eating or other aspects of diabetes. You may mean well, but giving advice about someone’s personal habits, especially when it is not requested, isn’t very nice. Besides, many of the popularly held beliefs about diabetes (“you should just stop eating sugar”) are out of date or just plain wrong.
- DO realize and appreciate that diabetes is hard work. Diabetes management is a full-time job that I didn’t apply for, didn’t want, and can’t quit. It involves thinking about what, when, and how much I eat, while also factoring in exercise, medication, stress, blood sugar monitoring, and so much more – each and every day.
- DON’T tell me horror stories about your grandmother or other people with diabetes you have heard about. Diabetes is scary enough, and stories like these are not reassuring! Besides, we now know that with good management, odds are good you can live a long, healthy, and happy life with diabetes.
- DO offer to join me in making healthy lifestyle changes. Not having to be alone with efforts to change, like starting an exercise program, is one of the most powerful ways that you can be helpful. After all, healthy lifestyle changes can benefit everyone!
- DON’T look so horrified when I check my blood sugars or give myself an injection. It is not a lot of fun for me either. Checking blood sugars and taking medications are things I must do to manage diabetes well. If I have to hide while I do so, it makes it much harder for me.
- DO ask how you might be helpful. If you want to be supportive, there may be lots of little things I would probably appreciate your help with. However, what I really need may be very different from what you think I need, so please ask first.
- DON’T offer thoughtless reassurances. When you first learn about my diabetes, you may want to reassure me by saying things like, “Hey, it could be worse; you could have cancer!” This won’t make me feel better. And the implicit message seems to be that diabetes is no big deal. However, diabetes (like cancer) IS a big deal.
- DO be supportive of my efforts for self-care. Help me set up an environment for success by supporting healthy food choices. Please honor my decision to decline a particular food, even when you really want me to try it. You are most helpful when you are not being a source of unnecessary temptation.
- DON’T peek at or comment on my blood glucose numbers without asking me first. These numbers are private unless I choose to share them. It is normal to have numbers that are sometimes too low or too high. Your unsolicited comments about these numbers can add to the disappointment, frustration, and anger I already feel.
- DO offer your love and encouragement. As I work hard to manage diabetes successfully, sometimes just knowing that you care can be very helpful and motivating.”
Introduction Tips
- Welcome and program overview: Briefly introduce yourself, the program, and the learning objectives for the session.
- Encourage participants to introduce themselves: Build camaraderie within your group through introductions (new participants) and re-introductions (prior participants).
- Make a list of the group’s curiosities: Encourage each person to share one thing they hope to learn in today’s session. Record each participant’s learning objective so each item can be addressed during the education session.
- Materials distribution: Ensure all participants have a copy of the Beyond Diagnosis toolkit. Today’s session will cover reference pages 42-49 for T1D Toolkit and pages 41-48 for T2D toolkit.
- Introduce your group to the Beyond Diagnosis ambassadors from Building Your Support Team
Education
Healthcare Team Building
The needs of each person with T1D and T2D are unique, and the healthcare team that supports each individual will be similarly unique. In this section, we introduce the diverse members of the healthcare team who can provide guidance and expertise. Receiving professional guidance from expert healthcare providers is one form of building a diabetes support team, though it likely shouldn’t be the only form of diabetes support that individuals with T1D and T2D have within their support team!
Primary Care Physicians (PCP)
Primary care physicians (PCPs) are knowledgeable in diabetes management and can be a valuable resource. Nurse Practitioners (NPs) and Physician Associates (PAs) are advanced practice clinicians who also assist in diabetes management and education.
Endocrinologist
Many people with diabetes prefer to consult an endocrinologist, a specialist in hormones who treats all types of diabetes. If one isn’t available locally, a primary care physician can also help. Endocrinologists offer specialized expertise, tools, and resources tailored to your symptoms and condition.
Diabetes care and education specialists
A Certified Diabetes Care and Education Specialist (CDCES) is your essential partner in managing diabetes care. They troubleshoot issues, identify health patterns, teach about and assist with diabetes technology, find cost-saving programs, and help answer any question you may have about diabetes or its impact on your body.
Mental Health Provider
Being diagnosed with diabetes means absorbing a lot of new information fast. Luckily, you can access mental health support through therapists offering video counseling or in-person counseling, including those experienced in diabetes management. Examples of mental health providers are psychiatrists, psychologists, social workers, and licensed professional counselors.
Pharmacist
A local pharmacist can guide you with new medications and monitor refills. They can also help navigate unexpected diabetes drug costs, acting as a valuable advocate. For assistance with insulin costs, visit GetInsulin.org to create a personalized access plan.
Clinical Pharmacist
Clinical pharmacists specialize in diabetes care, collaborating closely with patients to enhance their health. They are medication experts, crucially supporting the diabetes care team in dose management and medication scheduling for improved health outcomes.
Exercise Physiologist
Exercise physiologists specialize in developing personalized fitness plans to improve cardiovascular health, flexibility, and body composition.
Registered Dietitian Nutritionist*
A dietitian can assist by identifying which foods affect your blood sugar the most, planning balanced meals and snacks that are satisfying without restrictions, and ensuring your relationship with food stays positive and balanced.
*Not all nutritionists are Registered Dietitians
Neurologist
A nerve expert and specialist doctor who can be included as needed to treat nerve problems like extremity pain (from neuropathy).
Podiatrist
Foot specialist doctors who can be included as needed to take care of foot issues like ulcers or infections. Your primary doctor or diabetes doctor should perform a preventative foot exam once per year.
Optometrist
A local primary care eye specialist that can examine your eyes, check your vision, and identify any diabetes-related eye concerns.
Nephrologist
A specialist kidney doctor that can be included as needed to treat kidney problems like diabetes-related kidney disease. Your primary doctor or diabetes specialist should perform annual lab work to look after your kidney health.
Dentist
Dentists are experts in tooth, gum, and mouth health. Visiting your dentist is very important for oral health. Visit your dentist at least twice per year for cleanings and examinations.
Opthamologist
Specialist eye doctors who evaluate eye health and treat any vision problems, including any that require laser or surgery. It is common to see the eye doctor to monitor your eyes once per year for changes related to diabetes..
Upon diagnosis, each individual with T1D and T2D is thrust into a position of self-discovery and self-advocacy. Becoming confident in the individual’s patterns and challenges places the individual with T1D or T2D in a position of empowerment to make decisions about their care and health. This position may be unfamiliar to those in your group, but it is important to foster the idea that each person is the expert in their own body and can positively impact their long-term health with this engaged approach. The healthcare team is there to support, provide guidance, and medical management; however, each individual with T1D or T2D has an essential role as an active participant.
Nurturing positive healthcare experiences as an individual with T1D or T2D can be sensitive given that diabetes stigma and discrimination are prevalent in culture at large, but also exist in many care settings. Individuals with diabetes may need to evaluate their relationships with healthcare teams until they find providers who are supportive experts. Diabetes-focused peer communities commonly discuss supportive healthcare providers because finding care teams that sufficiently understand diabetes and provide non-stigmatizing care can be incredibly difficult. Even though it may require visits with multiple teams to establish a supportive relationship, this effort is worthwhile.
A supportive diabetes care provider says:
- I know managing diabetes isn’t easy—you’re working really hard.
- High blood sugars do not mean you’ve failed
- A healthy diet doesn’t have to be perfect—and it should include some of your favorite foods
- What kind of support would you like from me?
- What one part of diabetes management would you like to work on?
- Diabetes is really stressful—how are you feeling?
Adapted from BT1’s 6 Things Doctors Should Say to Patients with Diabetes
The T1D and T2D Toolkits (page 45 on T1D Toolkit and page 44 on t2 toolkit) provide a list of reflection questions let’s reflect on these together:
- Does the diabetes specialist spend enough time explaining what’s going on?
- Do you feel like you fully understand what they are explaining?
- The responsibility to be clear and understandable is on the healthcare provider. Are they acting like your partner in your healthcare journey?
- Are they recommending options you can try? Are they listening and asking follow-up questions when you’re hesitant?
Quiz Time
- Which diabetes expert can prescribe diabetes medications and review annual lab work?
- PRIMARY CARE PHYSICIAN
- Which diabetes expert is a specialty doctor with additional training in diabetes and hormones
- ENDOCRINOLOGIST
- Which diabetes expert can help navigate side effects from medications, assist with teaching you about new diabetes medications, and refill your diabetes medication?
- PHARMACIST
- Which diabetes expert can help troubleshoot diabetes care challenges, identify health patterns, teach about and assist with diabetes technology, and help you learn about any aspect of diabetes care or living well with diabetes?
- DIABETES CARE AND EDUCATION SPECIALIST
- Which diabetes expert can help identify which foods affect your blood sugar the most, plan balanced meals and snacks that are satisfying without restrictions, and ensure your relationship with food stays positive and balanced?
- REGISTERED DIETITIAN NUTRITIONIST
- Which diabetes expert can help develop personalized fitness plans to improve cardiovascular health, flexibility, and body composition?
- EXERCISE PHYSIOLOGIST
- Which physician expert can help keep your heart healthy by keeping an eye on your cholesterol, blood pressure, and family heart history?
- CARDIOLOGIST
- Which physician can help identify and treat any problems with your eyes?
- OPTHAMOLOGIST
- Which specialist doctor is a specialist in kidney health or kidney disease?
- NEPHROLOGIST
- Which medical professional looks after oral health and your teeth
- DENTIST
- Which specialist doctor is an expert in nerve function such as nerve pain?
- NEUROLOGIST
Taking Care of Your Mental Health
As healthcare providers, we know that diabetes is more than just numbers– It affects how people feel, think, and experience everyday life. Living with diabetes can be stressful and overwhelming given the hurdles of the current health care and health insurance environment. Diabetes distress, feeling burned out or overwhelmed by diabetes management, is very common but often overlooked. Those with T1D and T2D who experience anxiety, depression, and increased stress notice an impact on their blood glucose and know that these conditions make it harder to maintain self-care. Having a strong support system in place can improve health outcomes, happiness, and quality of life.
In this section, encourage participants to acknowledge the challenges of living with T1D or T2D, acknowledge their unique emotions about life with diabetes, and build a support system that feels positive. It’s important to emphasize that when our emotions are getting in the way of our self-care, it’s time to seek help from a mental health professional who understands diabetes. There are several resources in this module to help participants become aware of the impact diabetes is having on their emotions and how to get support from someone who can help.
4 of 5 adults with diabetes experience diabetes stigma and 1 in 5 experience diabetes discrimination. Diabetes stigma refers to exclusion, rejection, prejudice, or blame that people unfairly experience as a result of having diabetes. It affects people with every diabetes type, and can also affect their family members, too. They can be reinforced by anyone and anything such as medical professionals, friends, family and even those who live with T1D or T2D. Misinformation about diabetes can contribute to the belief that something you did caused you to get T1D or T2D. However, it is no one’s fault if they have diabetes. For years, people with diabetes have known how difficult it is to overcome many of the misconceptions about their condition and how society treats them as a result of having diabetes. Having diabetes is NOT anyone’s fault, and no one deserves to be treated worse because they have T1D or T2D.
- Unfortunately, there are many aspects of diabetes that are misunderstood in a cultural sense and these inaccuracies are harmful and hurtful to people with diabetes.
- Diabetes stigma and prejudice may result in worse self-care which can increase the risk for higher stress and worse health outcomes for people with T1D or T2D.
- It occurs in many settings like hospitals and doctors’ offices, schools and workplaces, places of worship and recreation, and social or personal environments, too.
This 2025 video illustrates the unique challenges of living with diabetes in today’s environment. The main character experiences diabetes, stigma and prejudice in several different settings- the workplace, at home, at the doctor’s office- until it builds to a point where he feels completely burned out from the demands of care and society’s perception of his lack of attempt at self-care. Acknowledging the challenge that diabetes stigma places on each person who lives with T1D and T2D opens new avenues to explore mental health. Despite the term “diabetes stigma” being relatively new, communities that support those with T1D and T2D, conversations about combatting misconceptions, building resilience, and becoming your own self-advocate have been commonplace for decades.
Open Discussion
Engaging the group to discuss their personal experiences with diabetes stigma within their journey builds camaraderie and similarities within the group. Though some group members may have been unaware of diabetes stigma prior to this module, many in the group will have experiences to share. Empower the group to share their experiences of what they have encountered, the impact it had on them, and how they moved forward. Allow time for peer-to-peer discussion; connection with others on this topic can be transformative.
- What are unhelpful things that others have said to you about diabetes or living with diabetes?
- What are the things that others have said to you that have HELPED make it easier to live with diabetes?
Emotional Check-In
Living with diabetes is complex, stressful, and can feel never-ending. It is important that participants check in on their stress, their emotions, and lean on their support networks when they need help. We all need help, and there are many different ways to get help- from friends, from family, from health care providers, from mental health experts, from the diabetes community… there is no wrong way to get help… as long as you get help when you need it!
Those with T1D and T2D are at increased risk for anxiety, depression, diabetes distress, diabetes burnout, disordered eating, fear of low or high blood sugar, challenges accepting diabetes, and difficulties taking or using insulin as recommended. Encourage participants to be on the lookout for symptoms of any of these mental and emotional concerns so they can be identified and treated proactively.
The American Diabetes Association recommends screening individuals with T1D and T2D routinely for psychosocial concerns such as diabetes distress, depression, anxiety, disordered eating, or cognitive dysfunction. Proactive communication with each individual and intervention is preferable to waiting until problems arise. If positive for behavioral health concerns, the care team should refer the individual with T1D or T2D to a behavioral health professional who has specialized expertise or who have received education about psychosocial and behavioral issues related to diabetes to ensure they receive quality, effective treatment. Although some individuals may not be comfortable seeking care for mental and emotional health concerns, your role as a trusted healthcare partner can increase the likelihood of a person accepting a referral for other services. Cognitive behavioral therapy and mindfulness-based interventions have been demonstrated as effective to treat psychological concerns and also can be effective in a preventative manner, as presented here in this module.
Situations that warrant a referral of person with diabetes to a behavioral health professional for evaluation and treatment
- A positive screen on a validated screening tool for depressive symptoms, diabetes distress, anxiety, fear of hypoglycemia, suicidality, or cognitive impairment
- The presence of symptoms or suspicions of disordered eating behavior, an eating disorder, or disrupted patterns of eating
- Intentional omission or underdosing of insulin or non insulin medication to cause weight loss
- A serious mental illness is suspected
- Low engagement in diabetes self-management behaviors, including declining or impaired ability to perform diabetes self-management behaviors
*adapted from Table 5.6 ADA Standards of Care 2025 Psychological Assessment and Treatment
Below are specific mental and emotional concerns for individuals with T1D and T2D. When available, there are links to validated, clinical screening tools to evaluate specific concerns (as recommended by the American Diabetes Association above). As an instructor, you have a critical role in educating your groups about these mental and emotional concerns for individuals with T1D and T2D. They will learn from your knowledge and example of what to do if these situations arise; encouraging participants to build their support networks and get care from a behavioral health expert if they need it is essential!
ANXIETY
Diabetes and anxiety go hand-in-hand. It is estimated that the prevalence of generalized anxiety disorder in those with T1D and T2D is 19.5%. Anxiety is worry that becomes overwhelming. People with diabetes may not be discussed very often, but research finds that it’s very common in those who live with T1D and T2D. 36% of people with diabetes struggling with anxiety will never receive treatment and support.WHAT DOES ANXIETY FEEL LIKE? Nervousness, restlessness, or feeling tense; Feelings of dread; Rapid heart rate; Fast breathing; Sweating; Trembling; Weakness; Difficulty focusing; Trouble sleeping; Strong desire to avoid things that trigger anxiety. The generalized anxiety disorder (GAD-7) screening is a validated screening tool that can be used to diagnose anxiety by a mental health professional. If anxiety symptoms begin to interfere with diabetes self-management behaviors, working with a mental health expert is the next best step.
- One in six people with type 1 diabetes (T1D) is affected by moderate-to-severe anxiety symptoms.
- One in five people with type 2 diabetes (T2D) who use insulin is affected by moderate-to-severe anxiety symptoms.
DEPRESSION
Approximately one in four people with T1D and T2D experience elevated depressive symptoms or depressive disorders. Research shows that if you have T1D or T2D, the risk of developing depression more than doubles. In fact, some studies show, that it could be as high as four times more likely to develop depression. People with depression have a higher risk of developing type 2 diabetes, and people with type 2 diabetes are more likely to develop depression after diagnosis. Levels of depression are highest in the months and the year immediately following the diagnosis of diabetes. Having severe depression is also a huge predictor of whether a person would develop diabetes-related complications. The diagnosis of a diabetes-related complication also increases a person’s risk of developing depression. Everyone at some stage of their life will experience “feeling down,” but depression is more than feeling “bummed out.” It’s a persistent feeling (lasting more than two weeks). Depression may cause people to stop doing things they used to enjoy; have trouble getting things done; find it difficult to focus; remain in their home for long periods; pull away from loved ones; or use alcohol or sedatives excessively. In addition to sadness, depression can cause feelings of guilt, anger, frustration, unhappiness, indecisiveness, and disappointment. The Patient Health Questionnaire (PHQ-9) can identify whether someone is experiencing depression and needs assistance from a behavioral health professional.
DIABETES DISTRESS
Stress from the demands of taking care of diabetes can be powerful and disrupting. Because managing diabetes involves continuous, daily tasks, diabetes distress is common in those with T1D and T2D. According to the American Diabetes Association, “Diabetes distress in people with type 2 diabetes is common and persistent, with prevalence rates over 60%. Among people with type 1 diabetes, the prevalence of diabetes distress is 22–42%, with a 9-month incidence of 54%” Diabetes distress is associated with higher A1c and skipped medications, poor nutrition, and being sedentary. Those experiencing diabetes distress have strong negative feelings about their diabetes care, feeling overwhelmed, angry, and frustrated about diabetes; They may feel controlled by diabetes or self-management routines; isolated; a need to avoid necessary diabetes management behaviors; or feel a complete lack of motivation to take care of diabetes because it all seems like too much. The Diabetes Distress Scale can identify if an individual is experiencing diabetes distress. It is important to note that experiencing diabetes stigma can cause diabetes distress. There are effective mental and emotional treatments shown to be effective at treating diabetes distress such as diabetes self-management training, cognitive behavioral therapy, mindfulness-based therapies, and motivational interviewing.
DIABETES BURNOUT
Diabetes Burnout is the manifestation of severe diabetes distress. When diabetes distress builds to an untenable amount, diabetes burnout occurs. Individuals experiencing diabetes burnout may feel completely “done” with diabetes. Diabetes burnout is a state in which someone with diabetes grows tired of managing their condition, and then simply ignores it for a period of time, or worse, forever thereafter. Unfortunately, diabetes burnout is common, and most people with T1D have experienced it at some point in their lives. It’s extremely important to work with a mental health specialist to navigate diabetes burnout.
DISORDERED EATING BEHAVIOR
Disordered eating behaviors are common in those with T1D and T2D and it is estimated that up to 20% of those with diabetes have some form of disordered eating. Eating nutritionally, balanced meals that provide adequate nutrition and maintain healthy blood sugar levels is important to people of all ages. Sometimes the emphasis on healthy eating to maintain healthy blood sugars for diabetes management can result in problematic eating behaviors that interfere with eating healthfully. Some of these eating problems can include: severe dietary restriction of certain foods or food groups, binge eating, night eating, feeling a loss of control over eating, becoming addicted to certain foods, or using unhealthy measures to lose weight quickly. Eating problems are serious and need treatment with mental health experts. Disordered eating can lead to poor health outcomes (increased A1c and risk for diabetes complications) for those who experience them, and they can make managing your diabetes even more challenging. The Diabetes Eating Problem Survey (DEPS-R) can identify disordered eating behaviors in those with T1D and T2D that need to be addressed by a behavioral health or mental health expert with training in diabetes.
FEAR OF LOW BLOOD SUGAR
Individuals with T1D or T2D may have preoccupying fears about low sugars that can disrupt many aspects of self-care such as medication administration, healthy eating, and physical activity. Fear of hypoglycemia affects one in seven people with T1D or T2D. Individuals with diabetes or their family members who experience this fear have a specific and extreme fear of the risk and occurrence of low or high blood sugar. Though a primary goal of diabetes management is to achieve healthy blood sugar levels while minimizing hypoglycemia, they can still occur for those taking glucose-lowering medications like insulin or sulfonylureas. A person with T1D or T2D may respond to their fear of low blood sugar by keeping their blood sugar levels (too) high, resulting in high blood sugar and future health problems from prolonged high blood sugar. When fear of low blood sugar begins to interfere with diabetes self-care (ie, taking less medication than needed, intentionally keeping blood sugars higher for prolonged periods of time), encourage participants to work with their healthcare team to understand the fear, address the cause, gain confidence in recognizing symptoms of hypoglycemia, have a low blood sugar treatment plan in place, and achieve health blood glucose results for long-term health. The Hypoglycemia Fear Survey (HFS-II W) can identify the concerns people with diabetes experience and the degree to which it presents a challenge to self-care that needs to be addressed with a mental health specialist.
FEAR OF HIGH BLOOD SUGAR
Similar to the fear of low blood sugar, the fear of high blood sugar is also possible in those with T1D and T2D. However, instead of the extreme fear being based around low blood sugar, the fear is rooted in what happens to the body during high blood sugar events. The fear of hyperglycemia may include fear of developing health problems (complications) from diabetes, not feeling confident in self-management, experiencing undesirable symptoms of high blood sugar, or a fear of DKA (severe high blood sugar which can be life-threatening). A person may respond to their fear of hyperglycemia by keeping their blood sugar levels (too) low, resulting in low blood sugar. Research shows that PWD tend to overestimate their risk for developing health problems from diabetes and that those who have this extreme fear are often experiencing extremely high stress, anxiety, and/or depression. Working closely with the healthcare team and mental health experts are the most effective treatment for overcoming these fears and living healthfully.
FACING LIFE WITH DIABETES
Adjusting to life with T1D or T2D involves acquiring new knowledge and developing daily self-management skills to manage a lifelong condition. Responses to T1D and T2D diagnosis are unique and different for each person: some people experience a range of negative emotions (e.g., shock, grief, anger, distress, or self-blame), while for others, the diagnosis has little impact, or can bring a sense of relief after a period of uncertainty about unexplained symptoms. The journey is different for everyone, but most people with T1D and T2D will need support from their health professionals, families, and peers at some point as they adjust to life with diabetes. However, if a participant is struggling to accept their T1D or T2D diagnosis and new self-care regimen, work with their healthcare team and a mental health expert with training in diabetes. Taking care of yourself is important for everyone, and avoiding self-care because life with diabetes seems too challenging is not a suitable long-term strategy. Understand that it is normal for this adjustment to feel unexpected, new, and uncomfortable but that others are there to support, listen, and guide as they become more comfortable. The power of this support from one’s support team can be life changing and exactly the kind of boost that’s needed to get through some of the more difficult seasons with T1D or T2D.
INSULIN USE
Sometimes the reality of starting insulin or needing more insulin to manage blood sugars can cause negative thoughts or feelings or a desire to avoid the insulin regimen altogether. There are many misconceptions about diabetes and about the use of insulin, which can be used as a stigma against people who need insulin to manage their blood sugar. This reality can create reluctance for many individuals with T2D to start insulin or add more insulin to a diabetes treatment plan, even when blood sugar results demonstrate that it’s needed. Individuals with T1D may resist the need to immediately start on insulin (knowing that other treatments exist for T2D) or be hesitant to increase their insulin doses (ie, to avoid weight gain or the misconception that their condition is worsening). Many people may have also experienced shame and blame for high blood sugar in their diabetes healthcare experiences and/or may have been threatened with insulin as a worst-case scenario (ie, “if you don’t get this under control, you are going to need insulin”). Research shows that around one in four people with T2D and that insulin is usually started later than clinically indicated for many individuals with T2D. report being “not at all willing” to start insulin. Because not getting the right amount of medication to manage blood sugar levels can lead to poor health, delaying insulin or not giving enough can cause poor health outcomes and increase the risk for diabetes-related complications. However, if someone in your group is struggling with adjusting to the idea of using insulin (ie, negative past experiences, fear of needles, lack of confidence in insulin’s effectiveness, fear of diabetes-related health problems once insulin is started, impact on self-perception and stigma/bias as someone who uses insulin, or fears about diabetes progression), it’s a good idea to slow down, help them get in touch with their healthcare team, and address hesitations with a plan. Mental health experts can provide important guidance to cope with the need for insulin and understand any root causes to fears, resistance, or avoidance of this necessary self-care task. The Insulin Treatment Appraisal Scale (ITAS) screening tool measures someone’s perceptions of insulin use which can uncover negative associations or behaviors that require additional discussion and intervention by mental health experts.
Getting Therapy
Receiving treatment for mental health concerns by attending therapy or counseling is critical for those who need it. Therapy can help individuals develop better coping mechanisms, improve self-esteem, make progress on their health journeys, and find relief from the chronic nature of long-term illness. Professional guidance from behavioral health experts like psychiatrists, psychologists, social workers, and counselors equips individuals with tools to manage ongoing challenges and adopt an optimistic mindset. As instructors, normalizing the experience of seeking and attending mental health counseling can improve your group’s openness to this support tool which is effective for managing stress, anxiety, depression, diabetes-distress, disordered eating, and other mental health concerns. Therapy improves the ability for many with T1D and T2D to follow their treatment plans and improve their overall quality of life.
Some hesitate to go to therapy because they believe it’s expensive or that they don’t “need” it because they should be able to work through challenges independently. There is also a stigma that you have to be “broken” to go to therapy, but that’s not true. Preventative mental health care is just as important as preventative physical health care.Therapy is a support tool that addresses messy and sometimes painful parts of life. Going to therapy will help the participant understand the science behind what’s happening, determine why certain emotions have emerged, and help develop a plan to move forward in a more positive way. Though therapy can be hard work, it is often a very worthwhile investment.
Therapy can be done in-person or virtually through telehealth. Each insurance plan offers different coverage or benefits for mental health counseling or psychotherapy. Many plans require a copay of $0-75 for the visit with a mental health expert. Locate the plan’s customer service on a health insurance ID card or websites to help find this cost information quickly. It is always possible to request a referral to a mental health expert from your healthcare team. Additionally the American Diabetes Association has a database of Mental Health Specialist with additional training in Diabetes
Peer Support at Home
BT1 and BT2 offer robust peer support communities. Encourage participants to join a BT1 or BT2 community online to connect with others living with diabetes. There are many people living with T1D or T2D engaged in peer support communities through the Beyond Type 1 and Beyond Type 2 community platforms. In-person community meetups are often posted on each community platform.
BT1 and BT2 Peer Communities
You can also find community online on social media by searching hashtags like #Type1diabetes or #Type2diabetes, or following Beyond Type 1 and Beyond Type 2 on social media.
Wrap Up Tips
- Journaling Prompt: Guide participants to write about their feelings regarding their mental and emotional wellbeing in their provided journals. On page 48 (T1D toolkit) and page 47 (T2D Toolkit), participants can complete the emotional check-in reflection page. This resource can be downloaded, printed, and used as many times as each individual needs during their journey. Encourage participants to create regular check-in points to evaluate how they are feeling about diabetes and the demands it places on their lives.
- Action Planning: Briefly discuss the importance of action planning and guide participants through the Discussion Guide for their Health Care Provider On page 49 (T1D toolkit) and page 48 (T2D toolkit), participants have a discussion guide they can use to obtain more information about diabetes during their next healthcare visit. Providing this template empowers participants with questions that they can ask their providers; some may feel intimidated to ask questions or not be confident in knowing questions to ask. This discussion guide and any material in the T1D or T2D toolkit can be used for inspiration and support during visits with the health care team.
- Next Steps: Although your time together as a group has come to an end, encourage them to dive in and learn more ways to connect with others in the community who understand the journey with diabetes and ways to raise awareness in your local community. Have them scan this QR code to join the Beyond Type 1 conversation on living with diabetes.

Section 5
Tap Into Community and Thrive Together
If you choose to provide this section as a support group or a virtual discussion, Instructors can seamlessly present the lesson using the BT1 and BT2 toolkits Tap into Community and Thrive Together section.
Otherwise, please connect your group to Beyond Type 1’s Community Guide and Community Apps found below: