The Negative Impact of Diabetes Stigma: “Words create reality”
Written by: Julia Flaherty
7 minute read
June 5, 2022
Key behavioral science research proves the impact of attitudes and words on people living with diabetes and why those stigmas must change.
Coverage of the American Diabetes Association (ADA) Scientific Sessions is brought to you by the ADA x BT1 Collab.
This coverage focuses on information shared in the session: “Stigma in Diabetes Care–Evidence and Solutions (With Richard R. Rubin Award Lecture).” Presenters included:
- Paula Trief, Ph.D. (State University of New York Upstate Medical University)
- Alan Delamater, Ph.D. (University of Miami Miller School of Medicine)
The first part of this session coverage focuses on findings presented by Jane Speight, MSC, Ph.D., CPSYCHOL, FBPSS.
The stigmas around diabetes are well-known to the people who live with it, but it is a real problem that needs to change.
Can health care professionals and people with diabetes change society’s perception of diabetes? Can spreading greater awareness and understanding change how those without diabetes talk about the disease?
Experts discuss proposals for actionable ways to eliminate the stigma problem that plagues the diabetes community.
Diabetes has image + language problems
“Diabetes, as a condition, has a real and pervasive image and language problem,” said Jane Speight, introducing her research.
Stigma is a “negative social judgment based on a feature,” Speight explained. “It can be experienced and perceived in many ways.”
“There are many sources of diabetes stigma, and therefore many impacts,” added Speight.
Fortunately, we can take steps to help reduce and eliminate stigmas that impact the diabetes community.
Speight shared several key statements that seem to resonate among people with diabetes:
- Diabetes has an image problem: It’s typically represented in the media by images of overweight or obese people. It’s portrayed unrealistically by unhealthy foods and sugary drinks. Very little attention is paid to other risk factors.
- Media stories often focus on people with diabetes being responsible for developing their condition and experiencing complications. Headlines use language to shame and blame people with all types of diabetes.
- Another key aspect of the image problem are common words society uses to describe diabetes. Those featured in the presentation included: “compliant, control, try, bad, irregular, risk, obese, failure, long-term, sufferer, unhealthy, adherence”—the list goes on! This unrealistic and harmful language fosters a negative emotional relationship for people with their diabetes and perpetuates misconceptions among the public.
- Diabetes language has many consequences: It can be distressing with a lasting emotional impact on people with diabetes, alienates and isolates (affecting diabetes self-care), and even affects health professionals—impacting attitudes and treatment advice. It contributes to burnout among all parties.
These statements contribute to one clear conclusion: The culture of blame and shame surrounding diabetes needs to end.
Where do diabetes stigmas come from?
To understand how to end diabetes stigma, we must know where it comes from.
Sources of stigma include the media, general public, colleagues, family, friends, and health professionals. Stigmas lead to stereotyping, blame, judgment, being treated differently, rejection and exclusion. Stigma can even foster self-stigma and shame.
In addition to the relationship between stigma and diabetes, the effects of stigma have been researched in other conditions like HIV/AIDS, obesity, mental health and epilepsy. Stigmas magnify social and economic inequalities.
Speight and her colleagues found ample evidence of stigma in the diabetes experience. She shared anonymous, poignant quotes from her qualitative research (that surveyed people with type 1 and type 2 diabetes) on stigma:
- “(Media campaigns are)…patronizing…hurtful…they’re telling the community that I gave myself the disease.”
- “I used to hide it from any boyfriends that I started to see…not everyone wants a sick girlfriend.”
- “I have had medical professionals say to me: ‘Well, it’s your own fault.’”
- “I didn’t even tell my husband. I told nobody. I actually felt so ashamed to have diabetes.”
The impact of diabetes stigma
Diabetes stigma can lead to the following in people with diabetes:
- Developing poor self-esteem
- Concealing, isolating and avoiding social activity
- Experiencing depression and anxiety
- Developing diabetes distress
- Adopting negative attitudes about people with type 2 diabetes who use insulin
- Not taking enough—or any—medication
- Not monitoring blood sugar levels enough or at all
- Persistently high A1c and blood sugar levels
- Avoiding the doctor and skipping diabetes check-ups
- Developing diabetes complications
- And more…
Even more alarmingly, Speight said, “The consequences of diabetes stigma may go beyond those for the individual to impact more pervasively for funding diabetes care, treatment and research.”
In other words, stigmas held by the health care and research community may prevent adequate funding and research in developing better treatments and care for people with diabetes.
This is a complex problem, which should spur a global call to action. More research, awareness and support is needed.
In an effort to help reduce stigma, Speight and her team created a series of videos for Australia’s national diabetes week in 2021 to encourage diabetes awareness, putting the viewer in the position of someone with diabetes.
Here is one of those impactful videos (that has almost 58,000 views to date):
Potential solutions focus on positive messaging
Speight said health care professionals tend to mistakenly believe that appealing to someone’s fears works better than encouragement. This is not the case.
While appealing to someone’s fears (i.e., “If you don’t do (this diabetes care action), you will lose (this part of your health).”) may motivate a person with diabetes, phrases like this will never encourage them in the positive ways they deserve.
There are harmful ways to motivate, and people with diabetes hear them too often. Appealing to a person with diabetes’s fears about their condition instead of encouraging them is a missed opportunity to reassure them they can thrive with diabetes.
Speight encourages that “gain-framing messages (are) more effective than loss-framing”:
- For example, it is the difference between asking a person with diabetes: “What will I gain by taking my medications and checking my blood sugar?” vs. “What will I lose if I don’t take my medication and check my blood sugar?”
When people with diabetes are encouraged instead of demonized, they gain emotional and mental health benefits. Solutions to end stigmas that prioritize empathy and support are what people with diabetes, the public and health care professionals need.
“Words don’t just reflect reality—they create reality,” Speight concluded.
Diabetes stigma can lead to many different negative health outcomes. If you have been personally impacted by diabetes stigma and need support, utilize these resources:
Related Resources
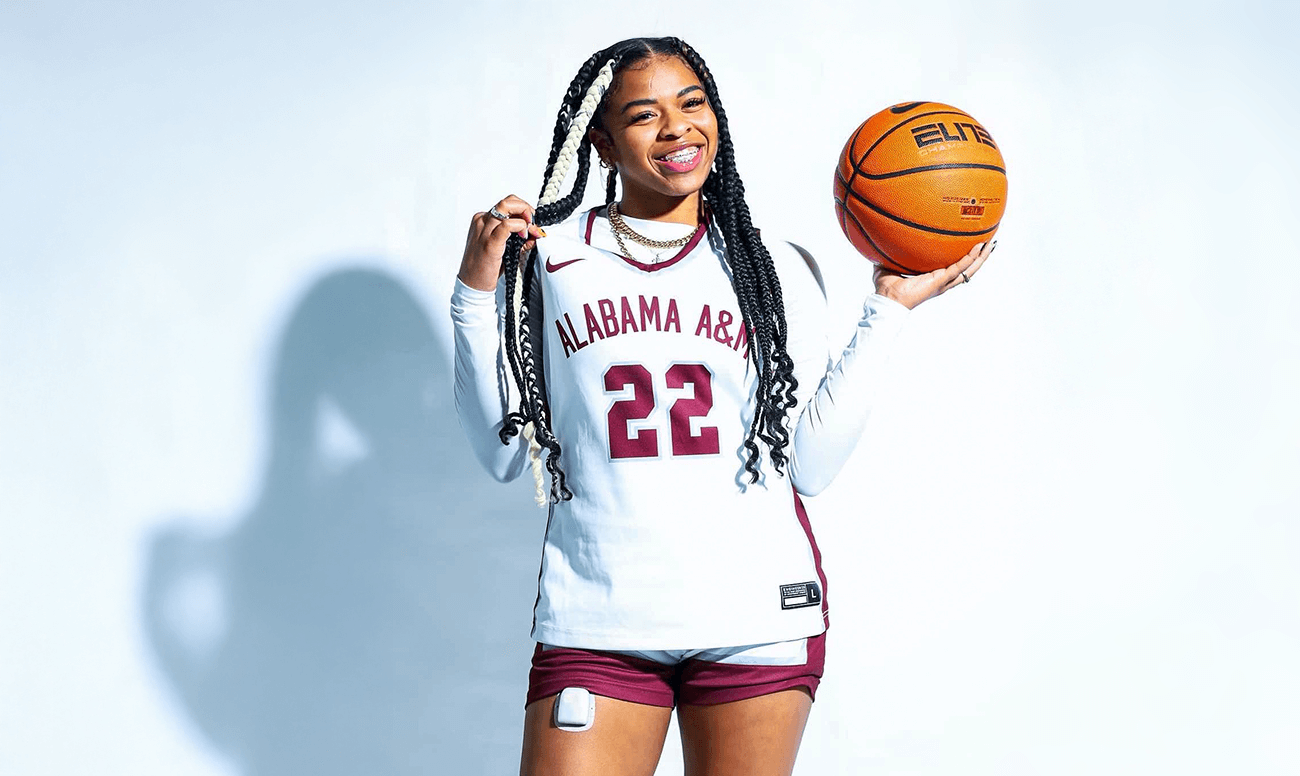
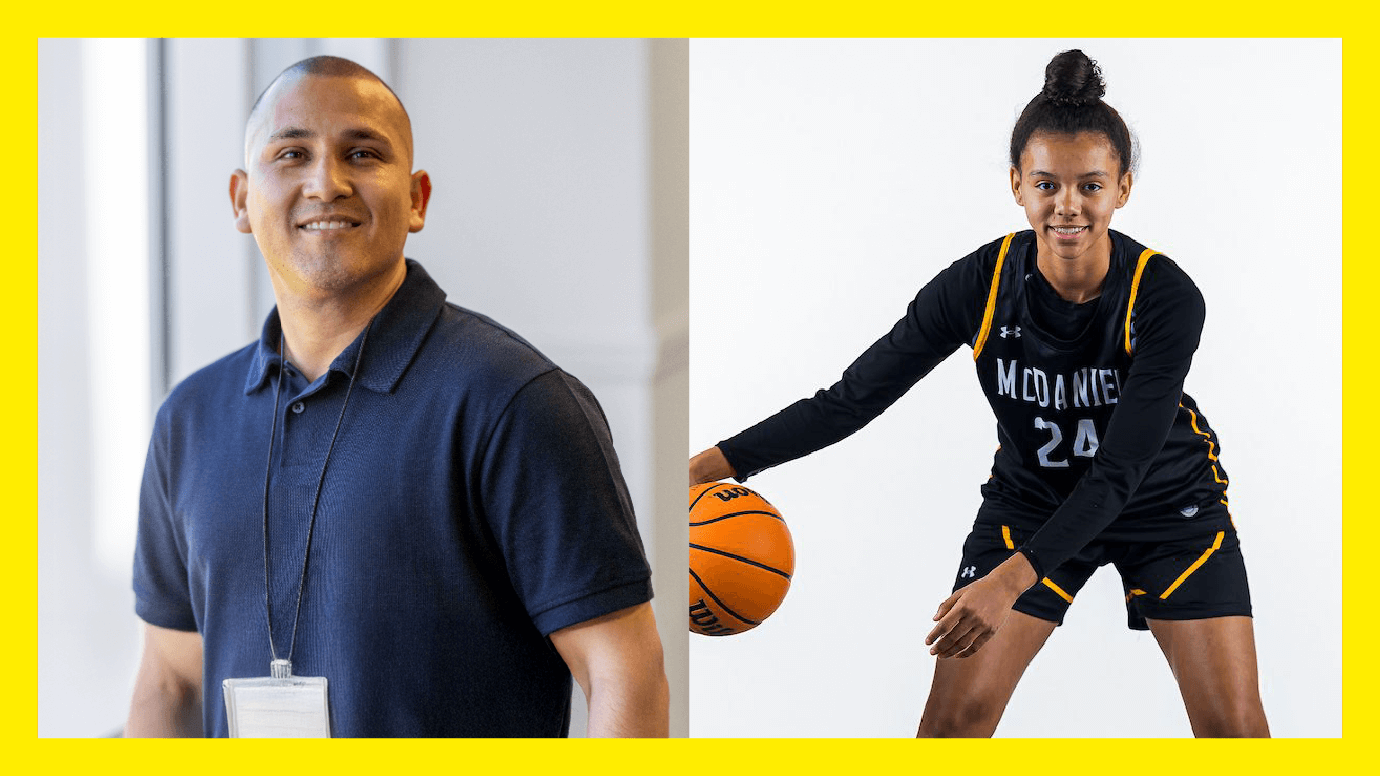
When 13-year-old Shelomi Sanders had a stomach ache, she never imagined it signaled a life-changing...
Read more
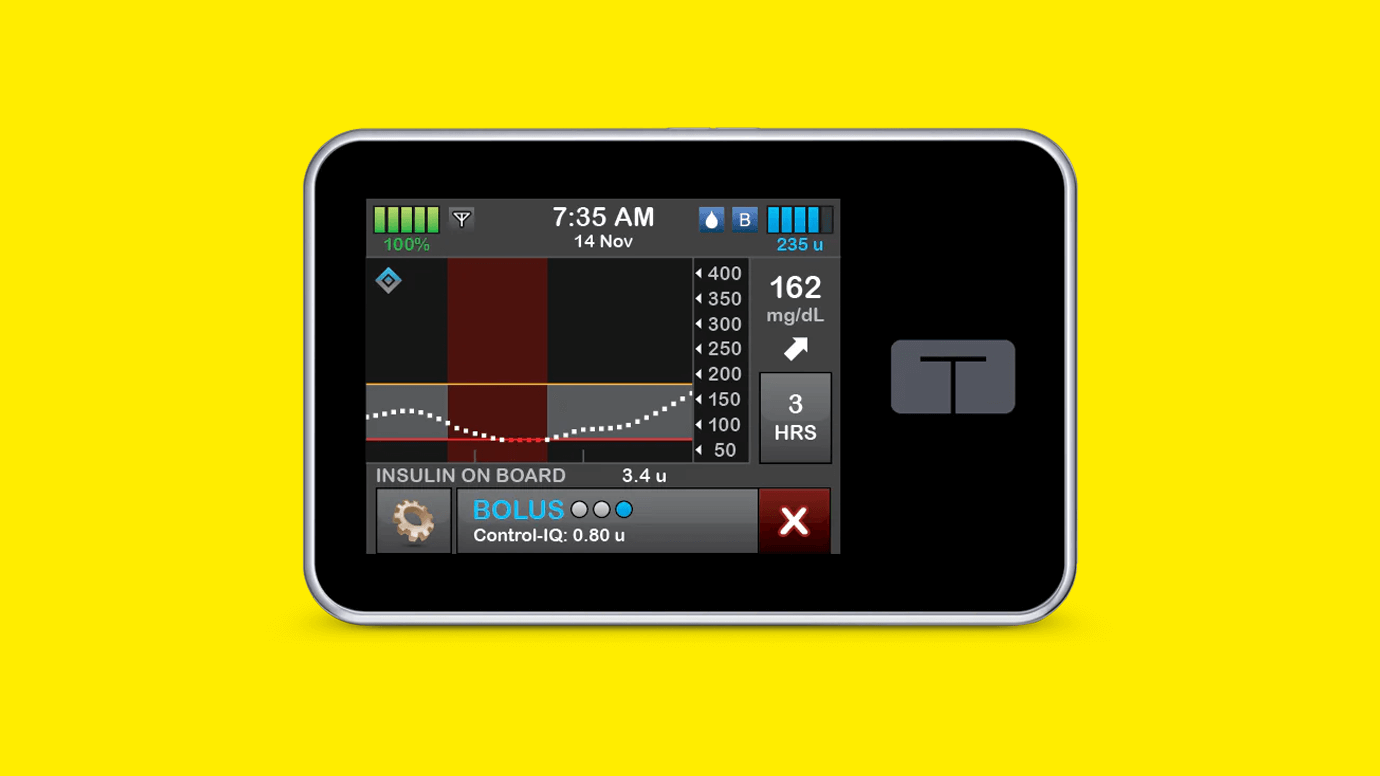
Big news for people with type 2 diabetes! Tandem Diabetes Care’s Control-IQ+ automated insulin delivery...
Read more

Jordan Chiles thrives on challenges, defying expectations, and excelling on the global stage. As a...
Read more