How an Automated-Insulin-Delivery (AID) System Transformed One Woman’s Mental Health
Written by: Daniel Trecroci
6 minute read
July 17, 2024
Beyond Type 1 interviewed Kiley Luckett, who has type 1 diabetes and uses the MiniMed 780G automated-insulin-delivery system, and Mark Heyman, PhD, CDCES, CEO of the Center for Diabetes & Mental Health.
This interview has been edited for brevity and clarity.
Beyond Type 1: I’m Dan Trecroci from Beyond Type One, and I’m grateful to be joined today by Kiley Luckett and Dr. Mark Heyman.
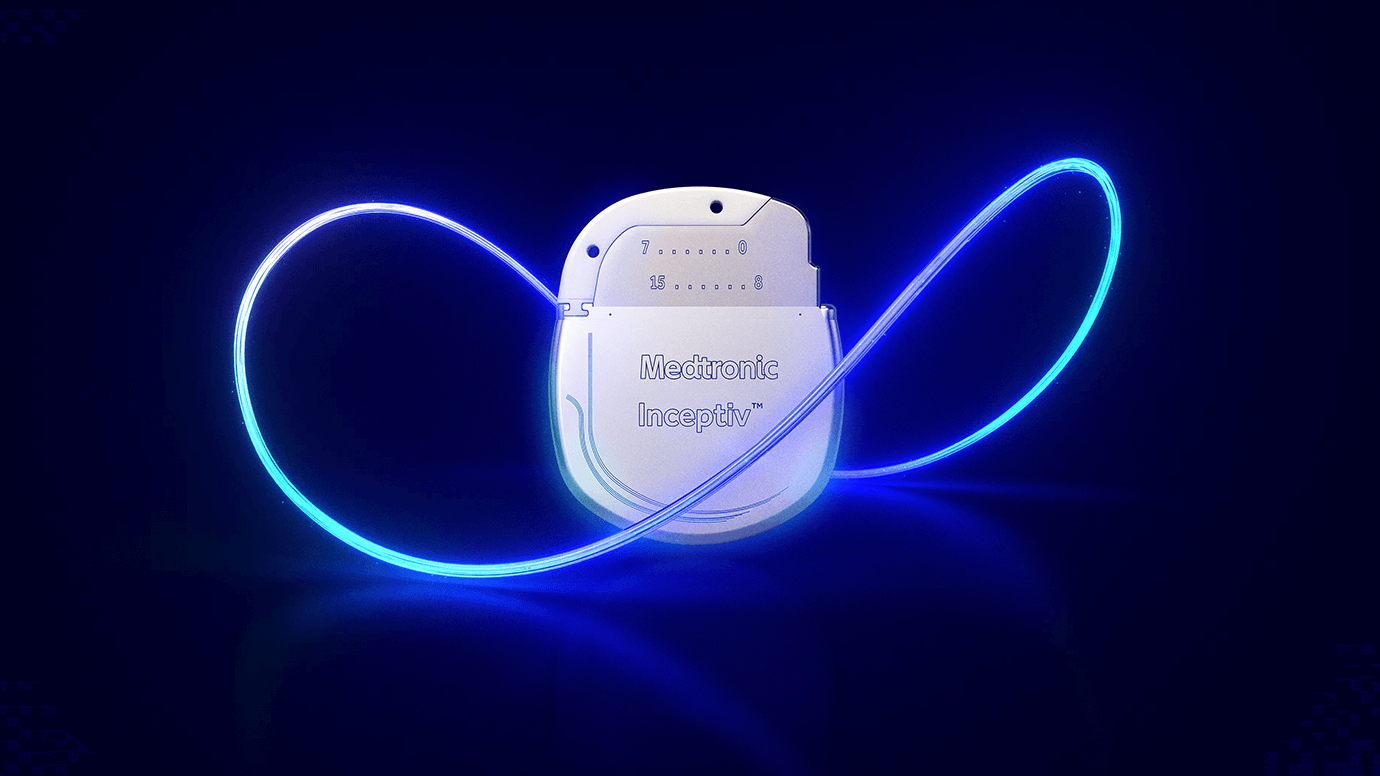
Kiley Luckett has type 1 diabetes and uses the MiniMed 780G automated-insulin-delivery system from Medtronic.
Mark Heyman is a CDCES and CEO of the Center for Diabetes & Mental Health. We’ll discuss how automated-insulin-delivery system like the Minimed 780G help with the mental-health aspects of living with diabetes.
Kiley and Dr. Heyman. Thank you for joining us.
Kiley Luckett: Thank you for having me. I love any opportunity to talk about automated-insulin-delivery systems and the MiniMed 780G. I love the advantages it’s had for my own mental health as a social worker.
Beyond Type 1: So, most people with diabetes know what insulin is, and they know what insulin pumps are. And, many people are starting to get an understanding of what a CGM is. What are we talking about when we mention an AID system?
Kiley Luckett: So, an AID system is a partnership. It’s how we bring the insulin pump and the CGM together to communicate and make choices. Based on the CGM readings and an algorithm, they communicate, and it will automatically adjust the insulin that you’re receiving based on lots of different factors.
Beyond Type 1: And are you wearing an AID system right now?
Kiley Luckett: I am. My CGM is on the back of my arm. There is the Guardian 4 sensor, and then the Medtronic 780G. It shows me that my sugar is sitting great at 87 right now, which is really cool given that I just had a piece of cake this afternoon. It shows that we’re sitting still in range and in a good place, because the CGM has talked with the insulin pump to give a little more insulin and then give a little less.
Beyond Type 1: So, you said you had a little bit of a cake. When it comes to indulgences like cake, how does the 780G differ from previous methods you have used to manage your sugar?
Kiley Luckett: With the older ways of managing diabetes, you would have a slice of cake, and your sugar would start to rise. That’s just what carbs do to each and every one of us—even the people who do not have diabetes. But, with my MiniMed 780G, as my sugar starts to rise, the Meal Detection technology would kick in. it would see that my sugar was rising, and that I don’t have any insulin on board. And so it’s going to start giving me microboluses to try to fend that off. So, while I might go over my ideal range, which is 180, I’m not going to be there for long, and it’ll bring me back down.
Several weeks ago, we had a pizza party at work. I had some pizza and realized maybe 45 minutes later that I forgot to bolus. I only went up to like 200 and I was back down in less than 30 minutes.
Beyond Type 1: You touched upon the Meal Detection technology, which is a signature feature of the MiniMed 780G. Are there any other 780G bells and whistles that you like?
Kiley Luckett: The 780G system with the Guardian sensor requires zero calibrations after insertion and the two-hour warmup period. Because of the initial two-hour warmup and subsequent six-hour calibration, I used to only start a sensor in the morning because I’m a busy—and occasionally forgetful—person. Now, I can change my sensor at any time—even at 8 p.m.—without worrying about being woken up in the middle of the night or going without a sensor if it falls off.
I consider the 780G my safety net. It helps manage my sugar levels by preventing extreme highs and lows, allowing me to focus less on constant decision-making about my diabetes.
Beyond Type 1: What type of compatibility does the MiniMed 780G have with smartphones? Is there an app of some kind that you have to use there?
Kiley Luckett: You don’t necessarily have to use the app, but it can be quite helpful. The app lets you see your data on your phone, and there’s also a partner app.
My husband uses it to get alerts when my sugar is low or high. Recently, while traveling, he noticed my sugar was low and alerted me. He also gets notifications if my sugar trends up at night, which helps him and gives me peace of mind.
The app shows your time in range, which is great for tracking your progress. Additionally, there’s a watch app, allowing me to quickly check my sugar during meetings without interruption.
Beyond Type 1: I want to talk to you and Dr. Heyman about mental health and diabetes. I’m interested in learning about your viewpoints regarding the psychological effects of living with diabetes.
Dr. Heyman: Type 1 diabetes is much more than a physical condition. It often involves significant psychological challenges as well.
Type 1 diabetes is a self-managed condition, meaning you—not your doctor—are responsible for your daily care. Managing Type 1 diabetes involves constantly making important decisions that affect your health, like what to eat; how much insulin to take; when—or whether—to exercise; how to interpret a glucose reading; how many carbs to take to treat a low; and more.
This responsibility can feel overwhelming.
Uncomfortable emotions are par for the course with type 1 diabetes. Living with a chronic condition can be challenging, and balancing everything necessary to live well with diabetes can be stressful.
Even if you do everything you are “supposed” to do, Type 1 diabetes can be unpredictable and frustrating. If you aren’t able to do everything you are “supposed” to do, it can cause feelings of anxiety, guilt, and even hopelessness. High sugar can also significantly impact your emotional state.
The emotional aspect of diabetes can affect how people show up in the world. For some, this means taking care of themselves and sticking to their diabetes-management plan. For others, it means feeling so depressed, anxious, or helpless that they have trouble going to work or school or doing things they enjoy.
Living with type 1 diabetes can also cause stress in relationships, making it hard to be a loving, supportive friend. It can also be a combination of these issues and other factors.
Kiley Luckett: I was diagnosed with type 1 diabetes in 1996 when I was in second grade, so I wasn’t very aware of my mental health at the time. I mostly remember the social changes that affected my mental health, like friends no longer inviting me to sleepovers because their parents were worried about my diabetes. This made me feel ostracized and different, wondering why I couldn’t just eat cake like everyone else.
As I got older, I rebelled. I didn’t take care of myself, skipped insulin doses, and lied to my doctors and parents because it was overwhelming. In college, I wanted to focus on my studies without constantly worrying about diabetes.
The turning point for me was discovering Medtronic in 2017. It made a significant difference in managing my diabetes. When I started using the latest CGM last year, I realized how exhausted I was from constantly monitoring my condition. It was like not knowing how sick you were until you got better. I had grown used to checking my sugar, adjusting my pump, and constantly thinking about what I could eat.
Learning to trust the new diabetes technology was a transition, but once I did, it made my life so much better.
Beyond Type 1: How has the evolution of technology— like AID systems and the MiniMed 780G—changed the mental-health “work” of living with diabetes?
Dr. Heyman: Automated- insulin-delivery systems have eased some of the mental burden of managing diabetes. Because these systems automate some aspects of insulin delivery, diabetes management now requires fewer decisions and less work.
They also reduce fluctuations in sugar, so people with diabetes spend less time and energy correcting out-of-range glucose levels, allowing them to focus on other important aspects of their lives.
Overall, AID systems help people more effectively manage their condition and with greater confidence.
Kiley Luckett: I used to struggle with the Dawn Phenomenon, where my sugar would spike every morning as soon as I got out of bed—even without eating. Starting the day with high sugar was draining. Now, I wake up with my sugar around 100, which feels great and helps my day start off right.
Additionally, managing my diabetes has become much easier, especially when on vacation. I don’t have to stick to a strict schedule for meals or insulin. I can sleep in, stay up late, eat, and fully enjoy life without constantly worrying about my sugar.
Beyond Type 1: You’re a social worker, right?
Kiley Luckett: I’m the director for mental health and social emotional learning for a school district.
Beyond Type 1: Before using the MiniMed 780G, what was it like working with students? And, how has your experience changed since transitioning to the 780G?
Kiley Luckett: That’s definitely a big deal. Working with kids in crisis, they don’t care about your sugar levels—you have to be present for them.
So, I often put my health on the back burner because I care about my students so much. The 780G helps me take better care of my students.
I also like the Guardian Sensor 4, which is approved for use on the back of the arm. I never used to wear sensors there, but now that I do, other students and people see them and say, “Hey, I have diabetes too,” or “My mom does,” or “I know what that is.”
It has been amazing to be acknowledged by other individuals with diabetes and to show them that we are not alone..
Beyond Type 1: Finally, I want to know how using an automated-insulin-delivery system like the MiniMed 780G has affected your daily routine and perspective on living with diabetes. What hope does it provide you for the future?
Kiley Luckett: It gives me so much hope. People talk about needing a cure for type 1 diabetes. While a true cure would be wonderful, this is pretty darn close, and I feel extremely grateful.
Related Resources

At just 17, Collin Lloyd is making a name for himself in karting—on and off...
Read more

Managing diabetes requires ongoing preparation. Organizing your diabetes supplies isn’t optional—it’s essential. Quickly locating insulin,...
Read more
Living with diabetes might be a pain in the neck, but diabetic peripheral neuropathy (DPN)...
Read more


