Rachael’s Story: My Stage 4 Diabetic Retinopathy Went Undiagnosed for Years
“I was diagnosed with retinopathy two years ago after a pretty significant hemorrhage in my right eye,” explains Rachael, who’s lived with type 1 diabetes for 27 years, since she was 4.5 years old.
“I was watching TV one night and this stick just jumped into my field of vision,” recalls Rachael. “At first, I thought it was a bug or a bit of fluff, but when I turned my attention to it, it moved along with my eye’s movements.”
 Rachael attempted to clear the spot in her eyes with eye drops, then washing her face—but nothing worked.
Rachael attempted to clear the spot in her eyes with eye drops, then washing her face—but nothing worked.
“So, I went to the emergency room to get it looked at. The nurses were all more concerned with my high blood pressure than what was happening with my eye, which I remember finding so ridiculous. ‘Tell me I’m not going to go blind and my blood pressure will come down!’ I said to them,” recalls Rachael.
“I’d also had a migraine all weekend, and they were quick to assume it was just related to that. We were there all night before a doctor finally looked at it and told me I had bleeding in my retina. They scheduled an emergency appointment with the nearby eye care center, and sent me home to rest before the appointment.”
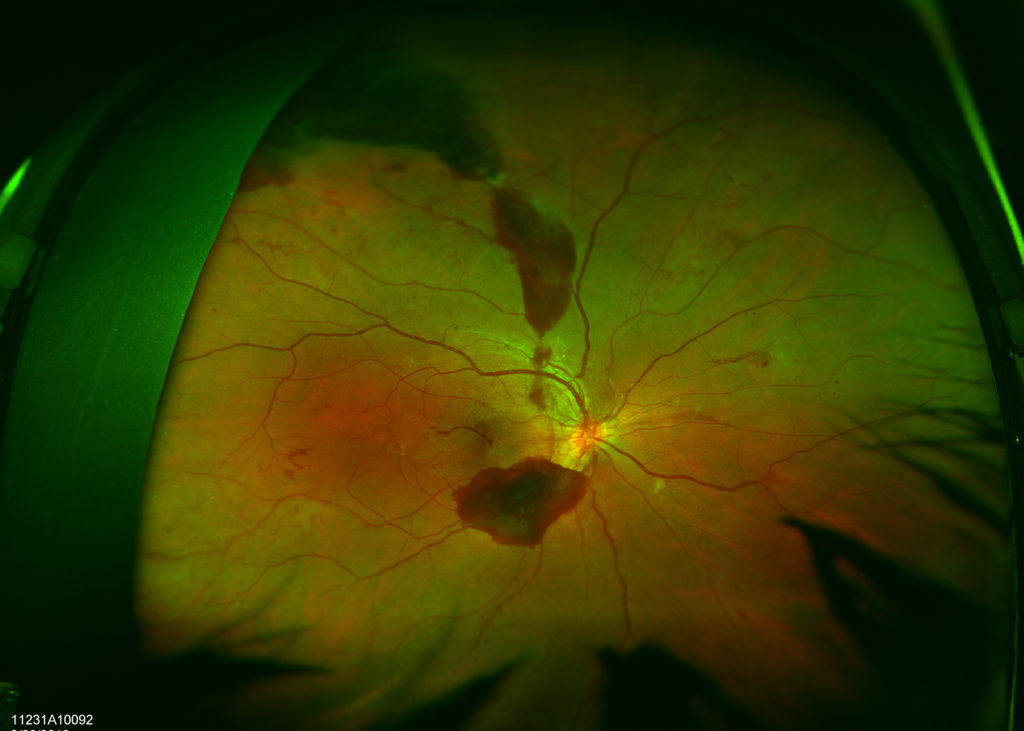
That morning, Rachael went through five hours of tests, injections of dye into her eye, followed by photos. Finally, they told her she had stage 4 retinopathy after years of gradual damage—none of which she had been aware of.
How did stage 4 retinopathy go missed for so many years?
Upon hearing she had stage 4 retinopathy, Rachael recalls bursting into tears because she had seen her eye doctor just three months before this bleed, and had never been diagnosed with significant retinopathy.
“Honestly, I have no idea how he missed it,” says Rachael. Looking back, she realizes he never did take photos of her eyes to look more closely at the retinas.
 “In my previous appointment, my doctor told me there was some mild bleeding, but nothing major, don’t worry, it would clear up on its own.”
“In my previous appointment, my doctor told me there was some mild bleeding, but nothing major, don’t worry, it would clear up on its own.”
Justifiably frustrated, Rachael missed several years of opportunity to treat those mild bleeders before they became something much more serious. Had she been properly diagnosed and treated, she could’ve likely kept her retinopathy in the earlier stages, rather than stage 4.
“Knowing what I know now, I wish I had demanded to be referred to a specialist immediately after hearing about those smaller bleeds,” says Rachael. “The other thing worth mentioning is that he was a regular optometrist, not an ophthalmologist. The only tests he did in office were using the auto-refractor, a vision test, and then dilating my eyes and looking at them with the lights and lenses.”
Rachael switched to a new optometrist who takes regular photos of her retinas to see the more critical details.
“And my retina specialist said I had years of damage. So, obviously, my first optometrist had missed a lot of signs of these issues, and could’ve helped me avoid all of this trauma.”
Starting treatments for stage 4 retinopathy
“My retina specialist decided to do an immediate round of laser treatments in both eyes to stop the bleeding and prevent further hemorrhages.”
Still battling a severe headache, Rachael recalls the bright lights throughout her many urgent exams, and feeling incredibly nauseous during that first laser treatment.
“The laser was an uncomfortable experience, but not really painful. It left me very sensitive to bright lights. When the laser was complete, I was told to come back in a month for another round of laser, and to see how things were doing.”
But the treatment didn’t prevent her next hemorrhage, which occurred only two weeks later in the same eye. Her retina specialist scheduled her for another urgent laser treatment two days later.
“We did the second round of laser that day, but that hemorrhage had completely blurred the vision in that eye. Luckily my left eye was completely unaffected at this point, so I was still able to drive, work and otherwise function normally,” recalls Rachael.
Just five days later, another small hemorrhage occurred, this time in her left eye.
Losing my vision
“At first, it wasn’t a big deal. But as time went on, my vision got worse and worse,” says Rachael.
 “As my work day went on, I was struggling to see the computer. I should not have driven home that day after the most recent hemorrhage. The fact that I made it home without hitting anything or anyone still amazes me to this day,” recalls Rachael, who admits she couldn’t see what color the traffic lights were.
“As my work day went on, I was struggling to see the computer. I should not have driven home that day after the most recent hemorrhage. The fact that I made it home without hitting anything or anyone still amazes me to this day,” recalls Rachael, who admits she couldn’t see what color the traffic lights were.
“I could barely see the car in front of me, couldn’t see oncoming traffic. It was terrifying. I somehow made it home, and again, burst into tears.”
The next day, her mother took her to an emergency appointment with the retina specialist to assess her overall vision.
“He told me, ‘Yep, you’ve definitely got a visual impairment’, and I decided on the way home that it was time to take a leave of absence from work.”
The process was going to involve a lot of paperwork to ensure she qualified for short-term disability, so Rachael called the retina specialist to confirm she’d have his support.
“His receptionist called me back later that afternoon and said, ‘Your doctor has no problem with that at all, since you’re seeing at the level of legally blind.’ I was shocked,” recalls Rachael. “He certainly hadn’t used those words when I was in his office.”
Living with low vision
Over the next few months, Rachael struggled both emotionally and physically.
“I was an emotional rollercoaster of worry,” she says. “Literally everything was a struggle at this point. Essentially I could see shapes and colors, but no detail. The best way I could describe my vision was if you smeared butter over the lenses of your glasses and tried to live with them like that…that was about as well as I could see.”
The vision in her left eye was slightly better than the right, which felt much like tunnel vision.
“Even if I was looking right at you, I might not have seen you,” says Rachael. “If we passed in a hallway, I probably didn’t see you.”
Rachael was unable to cook because she couldn’t measure properly or read labels, and her depth-perception was completely skewed, which meant managing insulin pen needles was also incredibly challenging. To cope, she started counting the clicks of the pen to measure her doses.
“Luckily I had the Dexcom at this point, and could easily read my blood sugars off my phone. I had to use almost all of the vision accessibility settings on my phone, and was surprised to learn that not all apps support your phone’s settings.”
She also struggled to see herself in the mirror.
“I had to stop wearing makeup and my hair was in a constant messy bun. If I dropped something or put it down on a similarly colored surface, it was unlikely I would ever find it again without assistance,” says Rachael.
And lastly, one of the hardest aspects of living with low vision that she didn’t expect was getting around in new places.
“Finding my way around places I didn’t know well was one of the hardest things, especially figuring out which was the proper bathroom to enter,” she recalls. “Unless the words ‘Men’ or ‘Ladies’ were massive, I had no idea which was which. When your vision is as bad as mine was, the little skirt on the sign for the women’s door basically blends in with the legs, they look identical.”
Overall, everything was affected—walking through the grocery store or through a crowd, reading price tags or sizes when shopping and even basic cleaning tasks at home.
“Basically, I completely lost my independence, which was really hard for me. I had to rely on everyone else for basically everything,” says Rachael. “Have an appointment? Need a ride. Want to see friends? Can’t meet them anywhere, they have to come to me. Want to go somewhere? Need someone to take you. Have to use the bathroom? Someone has to show you the way. I was lucky that I had a village of people willing to help and accommodate me, but it was still really scary, and I felt really alone in the whole process.”
My vision today: nearly back to normal
After two months of waiting for the blood to drain on its own from her three hemorrhages, Rachael received a vitrectomy to remove the lingering blood still blocking her vision.
Terrifying and stressful, she found the procedure to be far more emotionally tasking than painful, with only a mild three-day recovery period.
“Within a couple of days, I could tell my vision was already improving on that side. We waited a month before doing the vitrectomy on my left side, to allow the right side time to heal first and for me to finish all three of the prescription eye drops I had to take.”
Calmer for her second vitrectomy, it was a more complicated procedure because of extra scar tissue and a hemorrhage mid-surgery.
“But luckily within a month, that hemorrhage cleared up all on its own and no further surgeries were needed.”
With regular check-ups throughout the rest of the year, Rachael’s eyes have gradually healed and her vision has gradually improved. Today, she no longer needs regular appointments with a retina specialist and sees her new optometrist regularly.
Two years after the first bleed, Rachael’s vision is nearly back to normal.
This content on Eye Health was made possible through the ADA x BT1 Collab.





