Treatment Options for People with Painful Diabetic Neuropathy
Editor’s Note: This content was made possible with support from Nevro, an active partner of Beyond Type 1 at the time of publication.
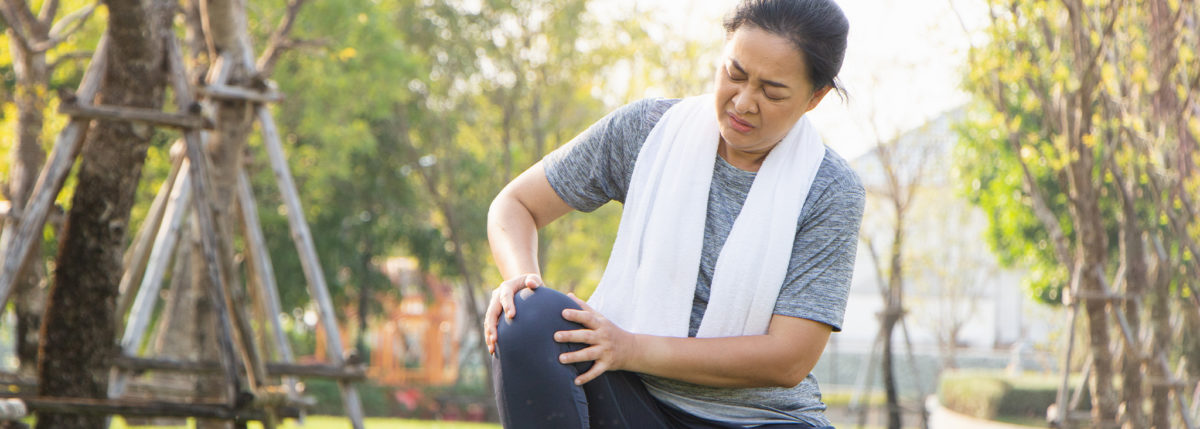
Overwhelmed by the severe pain of diabetic neuropathy? You’re not alone. More importantly, you shouldn’t have to suffer and endure that pain.
Diabetic peripheral neuropathy is considered the most common complication of diabetes, affecting approximately 30 percent of people with type 1 diabetes and 42 percent of people with type 2 diabetes.
The more advanced form of the complication is called painful diabetic neuropathy (PDN), characterized by symptoms including sharp pain, tingling and burning in your feet and legs. This diabetes complication eventually becomes impossible to ignore—and can have a huge impact on your quality of life.
While getting your blood sugar levels in a healthy range has proven to usually stop the progression of PDN in people with type 1 diabetes, the symptoms typically require a medical intervention to become more manageable. Finding the most effective treatment for your chronic pain is critical.
Here, we’ll look at the variety of treatment options for PDN available today.
Medications for Pain Management
Non-prescription pain medications: Acetaminophen (Tylenol) and NSAIDs (non-steroidal anti-inflammatory drugs: Advil, Motrin, Aleve) can be used for mild-to-moderate neuropathy pain. Acetaminophen works by actually blocking pain signals from being delivered to your brain, but it isn’t safe for regular long-term use because of its potential impact on your liver. (If you wear a continuous glucose monitor (CGM), it can also interfere with accurate blood glucose readings.)
NSAIDS can reduce pain by reducing your body’s overall inflammation. It does this by reducing your body’s natural production of the pain-inducing chemical “prostaglandin.” Like acetaminophen, NSAIDs are also not considered safe for regular long-term use because of their potential ability to cause ulcers, nausea and diarrhea. Using either of these non-prescription medications to treat your PDN should be discussed carefully with your healthcare team.
Duloxetine: Commonly known as Cymbalta, this medication is also prescribed to treat depression but has shown to be helpful in treating PDN, too. It reduces pain by actually increasing your body’s natural serotonin and norepinephrine production, both of which soften your brain’s experience of pain.
Gabapentin: Under the brand names Neurontin and Gralise, gabapentin is one of the most common prescription medications for diabetic neuropathy. It works by blocking the nerve’s signals of pain to your brain. It’s used to treat a number of other types of nerve pain because the side-effects are also generally mild. Usually taken at night, it usually comes with mild-to-moderate drowsiness. This side-effect can be helpful for those who have trouble sleeping through the night due to pain.
Opioids (narcotics): This class of highly addictive drugs (morphine, methadone, tapentadol, tramadol, etc.) can be used for severe PDN but only with careful supervision by your healthcare team. Considered a last resort due to the high risk of addiction, opioids are generally only recommended for “breakthrough pain” when treating neuropathy. The potential side-effects are extensive and can affect every part of your life if you become addicted and begin to abuse this drug with increased dosages and frequency.
Pregabalin: Originally intended as an anti-seizure medication, this medication is known best by its brand name, Lyrica. It works by blocking pain messages from traveling between your spine and your brain—even if the pain is in your feet and legs. Unlike duloxetine and gabapentin, this medication can be addictive and the side-effects are more noteworthy, including dizziness, drowsiness, confusion, swelling in your lower limbs and weight-gain.
Tricyclic Antidepressants: This class of antidepressants (including amitriptyline, nortriptyline, and desipramine) is different from those often prescribed for general depression and anxiety disorders. Used frequently to treat chronic pain, they work by increasing your body’s natural production of serotonin and norepinephrine, and they block pain messages coming to or from your brain. Side-effects can include drowsiness, dizziness, constipation and dry mouth.
Non-drug pain management options
Learn about the many non-drug pain management options that have been used to treat PDN in our deep-dive guide here, covering options including:
- Acupuncture
- Specialized footwear
- Supplements
- Exercise therapy
- …and more
Spinal cord stimulation technology
Spinal cord stimulation (SCS), first used to treat pain in 1967, is well researched and used across a variety of pain management cases. Compared to medication treatments for pain, these devices are not addictive and have no side effects like drowsiness, brain fog, or upset stomach.
HFX™ for PDN, is a Senza spinal cord stimulation (SCS) system that uses 10 kHz Therapy to treat pain from diabetic neuropathy. The HFX Solution, is the only SCS treatment option approved by the FDA to treat painful diabetic neuropathy, developed by a company called Nevro.
The Senza system is a small implantable device that is placed in your back just near your spinal cord during a minimally invasive procedure. That system is set to a specific frequency of 10kHz and sends small electrical pulses to your spinal cord. These pulses calm the nerves throughout your limbs and back. By calming those nerves, the system reduces the pain signals sent to your brain, reducing your physical pain.
According to research, about 80 percent of those who try the HFX Solution experience a significant reduction in their pain levels, and 90 percent of users keep using it. This technology is a “game-changer” according to many people with diabetes who are using it to manage their PDN pain.
Many users report no longer needing any other pain medications and are able to keep up with all of the physical activity they want and need to do throughout the day. For those who want to try it, there is an initial seven-day trial you will undergo to see if it’s right for you. You can start here with this basic online assessment to further determine if this technology might be a good fit for you.
Potential side-effects: After the out-patient implantation surgery, there is a low risk of infection or bleeding at the implantation site. There are no ongoing or long-term side effects.
The Bottom Line
You do not need to suffer through the intense daily pain of neuropathy. While it can take some time to find the right treatment to help you manage and reduce your pain, there are new and better treatments available today. Talk to your healthcare team about finding the right treatment option for you!