What is the Difference Between Mealtime Insulin and Long-acting Insulin?
Written by: Kourtney Johnson
4 minute read
May 2, 2024
Have you begun taking insulin at mealtimes? Has your physician discussed it with you? You may be wondering how the numerous types of insulin on the market differ from one another. Read on to learn about the differences between mealtime and long-acting insulin.
What is the Difference Between Mealtime Insulin and Long-acting Insulin?
Sometimes referred to as “background insulin,” long-acting insulin is used to maintain stable blood-sugar levels.
“Basal insulin is 100% meant to be for the glucose that your liver naturally produces,” says Jennifer Okemah, a registered dietitian and certified diabetes care and education specialist. “Your liver is constantly releasing glucose, and so the design of the basal insulin is just to keep up with liver production.”
On the other hand, mealtime insulin is designed to compensate for the increase in blood-sugar levels that occurs with food.
Consider it this way:
- The glucose that you eat provides your body with “fuel.”
- Long-acting insulin is necessary to help transfer this fuel from the bloodstream into the cells
- Your body can then use it as energy when you have diabetes and your beta cells are malfunctioning.
- Mealtime insulin’s role is to quickly lower blood-sugar levels during a meal.
- Mealtime insulin can:
- Begin operating in as little as 15 minutes
- Reach its peak in one to two hours, and
- Operate for approximately three hours in total.
Okemah says that the pace at which insulin works is still too slow.
“It’s the limitation of our medications,” she says. “Our rapid-acting insulins are not fast enough. I’m so frustrated by that because we have all of this beautiful technology that just keeps getting better and better, and we’re still fighting the timing of when the insulin works.”
What Are the Benefits of Mealtime Insulin?
There are a few advantages to taking mealtime insulin.
- The first is that eating at mealtimes most closely resembles what would happen if your body could make insulin.
- The second is that you can have meals and snacks at different times each day as long as you take your insulin 15 to 20 minutes before you eat.
Okemah states another major advantage of mealtime insulin.
It provides energy.
“Anytime you poke your finger or look at your continuous glucose monitor and the blood-sugar levels are high, that means that the fuel [glucose] is trapped,” says Okemah. “The fuel has to get ‘untrapped’ and there’s a few ways to untrap the fuel. The most physiological way is with insulin.”
Okemah adds that insulin acts similarly to oxygen in the body, allowing glucose to enter each cell and provide enough energy to get through the day.
“Insulin is not a failure,” she says. “It’s not a punishment. It is a physiological necessity. Whether your body produces its own insulin or you have to get insulin into your body using technology, it is a necessity either way.”
How to Calculate a Starting Dose of Bolus Insulin for Meals
There are ways to calculate a general starting dose of both basal and bolus insulin.
Work with your healthcare provider to determine what your individual needs are.
When starting mealtime insulin, it is typically assumed that one unit is given for every 15 grams of carbohydrates you eat.
The standard method for calculating the amount of insulin required to lower blood sugar is to assume that one unit will lower blood sugar by 50 points.
Assume you consume 55 grams of carbohydrates and your blood-sugar level is 204 mg/dL prior to eating. Using the tables below, you can calculate how much insulin you would need.
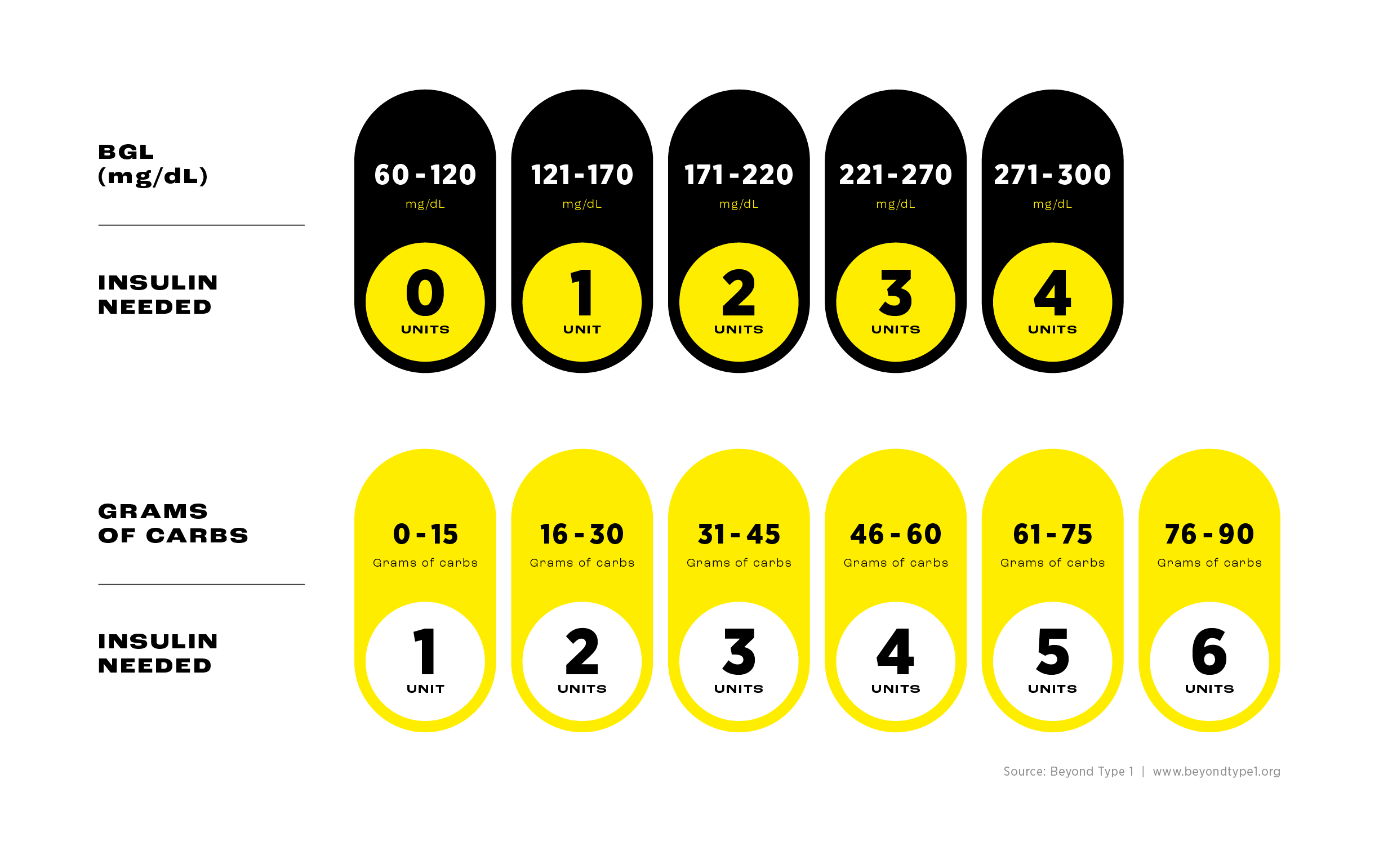
In this case, you would require two units of insulin to lower your blood-sugar levels and four units to make up for the fifty-five grams of carbohydrates—for a total of six units of insulin.
Okemah clarifies that medical professionals—using specific formulas—can calculate your insulin-to-carb ratio, which is the quantity of short-acting insulin required to control your carb intake during a meal or snack.
Furthermore, your body uses insulin differently in the morning and evening, and occasionally the ratio of insulin to carbohydrates varies during the day.
How to Calculate Your Basal Insulin Dose
According to Okemah, figuring out your body weight in kilograms is a good place to start when figuring out your basal dose.
You can do this by dividing your weight in pounds by 2.2.
Ex: 190 pounds/2.2 = 86.36 kilograms
Most people need between 0.2 and 0.5 units of insulin per kilogram of body weight.
So, if you weigh 190 pounds, multiplying 86.36 (your weight in kilos) by 0.2 yields a conservative estimate.
Ex: 86.36 x 0.2 = 17.27 units
Speak with your healthcare professional to further establish the appropriate dose for you.
Evidence of Safety and Efficacy When Titrating Insulin
To achieve your target A1C, you must titrate—or increase—your insulin dosages, which are typically low when you first start therapy.
Your physician can determine how much and how often to increase your insulin using a variety of calculations.
Research has demonstrated that it is both safe and effective to increase insulin dosages based on an individual’s needs.
Get Support
It is critical to keep in mind that insulin is only a drug—or a tool—to help you better control your blood-sugar levels. You have not “failed” because you need to take it.
Making a connection with others who are experiencing similar things can be very beneficial at times.
Joining the Beyond Type 1 Community is a great option if you want to connect with people who share your experiences!
Related Resources

The holiday season is filled with celebrations, family gatherings, and plenty of holiday foods. No...
Read more

Managing diabetes is a complex and often overwhelming journey—even nine years after my daughter's diagnosis....
Read more

The holiday season is all about celebration, family, and joy—with a little chaos sprinkled in...
Read more


