Fighting For a Type 1 Diagnosis: Vincent’s Story
Written by: Lala Jackson
5 minute read
March 23, 2022
Editor’s Note: Get involved in Beyond Type 1’s #SeeTheSigns of diabetes campaign! Share your signs to help save lives, request #SeeTheSigns posters to share in your community, get sharable graphics for social media and more! Learn more here.
Are you an adult navigating a recent type 1 diabetes diagnosis? Our partners at JDRF created the free No Limits Adult Care Kit just for you—packed with information and tools to educate, support and inspire newly diagnosed adults with type 1 diabetes (T1D). Request yours here.
For the six months before an emergency room staff almost sent him home with a blood sugar reading over 900 mg/dL, 25-year-old Vincent Carter had been feeling less and less like himself. Based in Bellingham, Washington, he was used to an active lifestyle, but he had started feeling like he never got the rest he needed at night.
Every step felt heavy, like he had sandbags around his waist, and he was constantly thirsty and insatiably hungry, like his body wasn’t getting any nourishment or hydration. He didn’t understand why his vision would become blurry some days. “I felt like all the things I was normally able to do, my body was letting me down. It just couldn’t do it,” Vincent says.
During a visit to his family’s home on San Juan Island, Washington in October 2021, Vincent’s mom Alexis became worried. Remembering Beyond Type 1’s Warning Signs campaign shared by her friend and fellow San Juan Island resident Sara, chief creative officer for Beyond Type 1, she knew she had to check in about his symptoms.
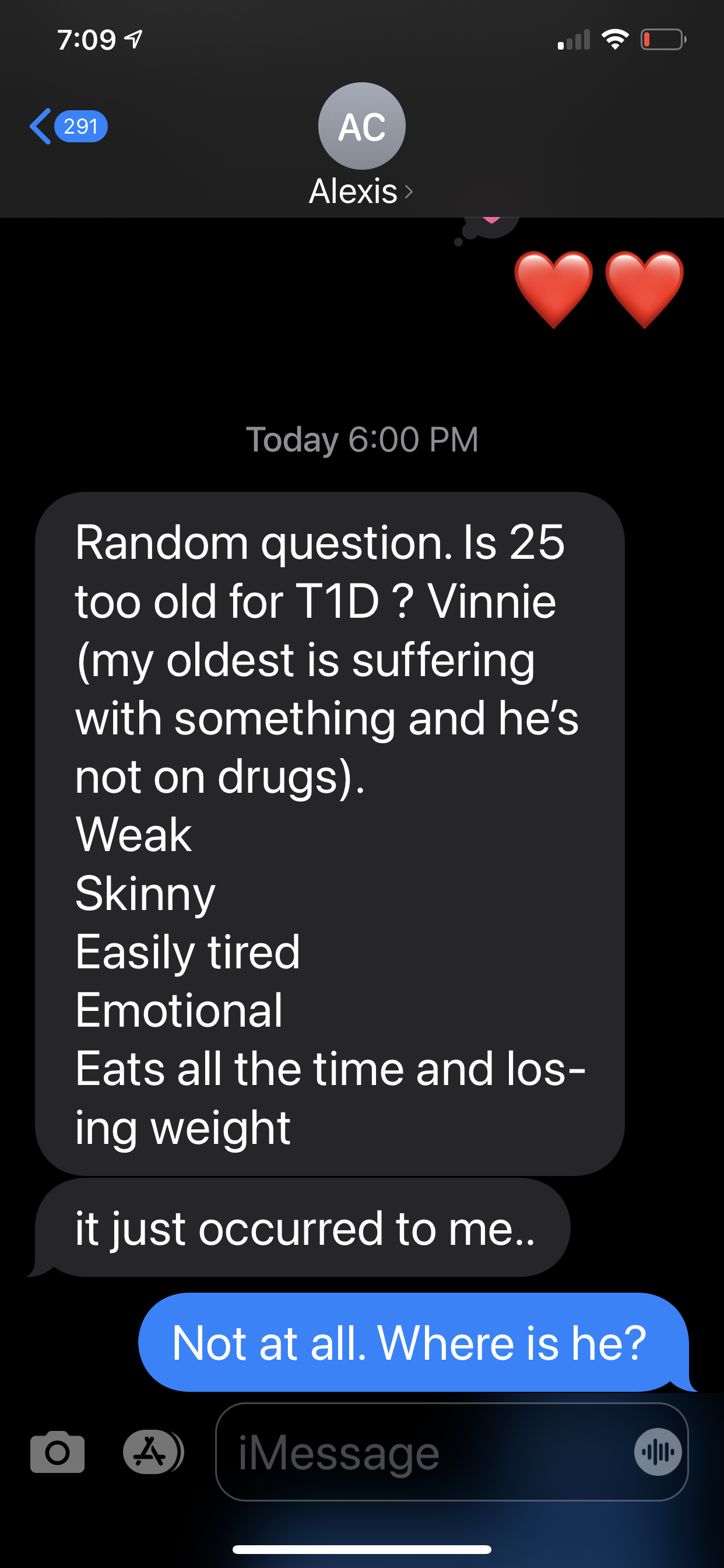
A text from Vincent’s mom Alexis to Sara, asking about Vincent’s symptoms.
The rush to get Vincent emergency care
After finding out Vincent was at his brother Chase’s house, Sara told Alexis she was on her way, rushing from her son Henry’s soccer practice. Henry, who lives with type 1 diabetes, changed his blood sugar testing kit’s lancet in the car on the way.
As soon as they reached Chase’s house, Sara walked into the open garage where Vincent was hanging out and asked to check his blood sugar. “HIGH” was all the meter read. Sara asked Vincent to wash his hands, but on a second check, the meter had the same reading. A blood ketone meter check also read high. “Pack your brother a bag,” she said to Chase. “We need to go to the emergency room right now.”
Living in a small island community, Sara had already had a few run-ins with the emergency room staff, including one time when they refused to give Henry fluids when he had high ketones after an insulin pump malfunction, ultimately sending him into diabetic ketoacidosis (DKA). While Sara had been able to get Henry the care he needed eventually, she knew she was going to need to be insistent for Vincent.
“I think that my friend here has undiagnosed type 1 diabetes,” she told the nurses. She showed them the meter readings from Vincent’s blood sugar checks. The nurse looked at Sara and asked if Vincent had taken insulin that day, but Sara reminded the nurse that he hadn’t been diagnosed. “Well, how do you know that he has it?” the nurse asked.

Vincent, 3 weeks before his diagnosis
Sara reiterated, “His blood sugar is reading ‘high’ on this meter. My son has type 1 diabetes. so I do know a bit about this.” The staff took Vincent into the ER, but Sara noted that they didn’t seem too worried about the situation. After about 30 minutes, a doctor came out to the waiting room, where Sara had been joined by Vincent’s mom Alexis. “We’re giving him some IV fluids. He’s dehydrated,” the doctor said. Alexis told Sara that they’d be okay there and that Sara should go home.
“As soon as I got home, I got a really bad feeling,” Sara says. “So I packed some food and books for Alexis and one of my Freestyle Libre CGM [continuous glucose monitor] sensors for Vincent and headed back to the ER.”
Fighting the discharge that could have killed Vincent
Shortly after Sara returned, an ER staff member told them, “We’re going to discharge him.” After asking why, the staff member said, “We can’t take care of him here. He can either go home or he can go to an emergency room off-island.” Late at night, there were no more ferries off-island for the evening.
But Vincent’s blood sugar was still over 900 mg/dL, having received no insulin, only saline to try to rehydrate him. After having the staff ask Vincent’s permission, Sara went to Vincent’s room to see how he was doing. Because his blood sugar was still so high, he wasn’t feeling well. Sara asked the doctor to confirm Vincent’s blood sugar and confirm that he had high ketones.
“So he’s going to go into DKA,” Sara said.
“No, I don’t think so,” the doctor replied.
Sara was flabbergasted, but the doctor reiterated that they couldn’t take care of Vincent at the ER. Sara asked to talk to the doctor in the hallway, where she was clear with him, “He’s going to die. He’s literally going to die.” But the doctor walked away. So Sara walked back into Vincent’s room and placed the Freestyle Libre CGM sensor in his arm, telling him to download the app that came with it and text her with his blood sugar every time he scanned the sensor. “Do not leave this hospital bed,” she told him.
Frustrated with the lack of care Vincent was receiving, Sara sent a text to Thom, Beyond Type 1’s late CEO, explaining the situation. “WTF?! Let me text Fran,” he messaged back, asking for the number of the emergency room. Dr. Fran Kaufman, chair of Beyond Type 1’s science advisory committee, immediately called Sara to ask a few questions about the situation, then hung up and called the ER.
Within thirty minutes, the previously unbudgeable doctor walked back into Vincent’s room. “So I just got off the phone with Dr. Kaufman and it looks like we are going to be admitting Vincent. And he likely has type 1 diabetes,” she said. “He is going to need to start insulin immediately. And we can’t discharge him at this time.”
Vincent ended up staying at the ER overnight to stabilize. Using the CGM, he sent Sara his blood sugar readings every hour until he fell asleep. A few days later, Dr. Kaufman was able to get Vincent an appointment with Dr. Ehrnhardt and her team at the University of Washington Diabetes Institute Clinic.
“I was fortunate to have my friend there to advocate that I really needed more attention,” says Vincent. “I was hooked up to IVs, but it took about 12 hours for them to be able to start giving me insulin. I have a couple of memories of waking up in the night with muscle spasms in my legs, so they gave me potassium too.”
Processing his diagnosis
“The next few days after I was diagnosed, I thought the world as I knew it was over,” Vincent says. He thought he had to eliminate all carbohydrates from his diet, and didn’t yet understand the role of injecting insulin.
Having lost about 45 pounds, it took some time for Vincent to get back to his new normal, but “since then I feel supercharged,” he says. He’s learning more every day about how diet and exercise impact his body.

Vincent, several months after his type 1 diabetes diagnosis
“Looking back, it’s hard to believe I kept convincing myself I was fine,” Vincent says. “Despite a couple of people commenting on my weight and low energy in the weeks leading up [to my diagnosis], something like diabetes wasn’t even a thought. That’s why I believe in increasing awareness. No one should have to get really sick to receive a diagnosis, it can be caught earlier.”
“There are a lot of good days but when [my blood sugar is] out of range, I can beat myself up for it sometimes. I’ll always be working on that. I want to live as another example that someone with type 1 can not only survive but thrive.”

Author
Lala Jackson
Lala is an author and communications strategist who has lived with type 1 diabetes since 1997. She worked across med-tech, business incubation, library tech and wellness before landing in the type 1 diabetes (T1D) non-profit space in 2016. A bit of a nomad, she grew up primarily bouncing between Hawaii and Washington state and graduated from the University of Miami. You can usually find her reading, preferably on a beach.
Related Resources

The holiday season is filled with celebrations, family gatherings, and plenty of holiday foods. No...
Read more

Managing diabetes is a complex and often overwhelming journey—even nine years after my daughter's diagnosis....
Read more

The holiday season is all about celebration, family, and joy—with a little chaos sprinkled in...
Read more


