The Wearable that Changed My Life
Editor’s Note: This post originally appeared on Medium and is being shared with permission.
A note from the author: Please do not interpret this post as medical advice. Everyone is different and the changes I made might not work, or might even be dangerous, for you. Consult your healthcare provider before making any changes to your diet, medication or any other part of your routine.
How a continuous glucose monitor got my A1C down to 5.8%
Introduction
As of this year, I’ve been a person with type 1 diabetes for 18 years. And I’ve never felt as good as I do today. What got me here was made possible by a small circle-shaped sensor placed on my arm called a continuous glucose monitor, but let me back up and start from the beginning.
When I turned 20 years old, I was doing military service in the Swedish navy and for a couple of months I had been feeling pretty bad. I was dehydrated, I had to go to the bathroom ten times a day on average and I had terrible mood swings. I thought I was suffering from an extended cold until I met the navy doctor. After listening to my symptoms, he decided to prick my finger and check my blood sugar level. I think I remember it being around 500 mg/dL (normal is 90) and the doctor said: “We have to take you to the hospital.” I was diagnosed with diabetes.
The Freestyle Libre sensor from Abbott:
The complexity of diabetes
Diabetes is often mischaracterized as a single disease when it really describes a set of symptoms that can have multiple different causes. Traditionally we’ve divided patients into two categories: type 1 and 2, or juvenile and adult, but some new research has emerged suggesting there are five different clusters with slightly different characteristics. In this new categorization, I’d be in the “Severe Autoimmune Diabetes” camp which is the most severe form of the disease.
Diabetes is a disease that, due to the lack of insulin, prevents your body from processing glucose (a simple form of sugar used as fuel in your body) which results in elevated levels of it in your bloodstream. Over time, high glucose in your blood will damage your organs and lead to cardiovascular disease, stroke, blindness, kidney failure and heart attack. For people with the condition, this means having to inject insulin on a daily basis to try and make sure your body gets enough to cover things like food.
As a person with diabetes, you have a wide range of tools that help you manage your blood-sugar levels at any given moment: syringe pens filled with injectable insulin, a blood-sugar meter, glucose tablets and more. Managing your blood glucose levels is not only about preventing highs; as a person with type 1 diabetes, you also risk taking too much insulin resulting in dangerously low blood glucose levels which can lead to a coma and even death. It’s a delicate balance that every person with diabetes has to manage closely on a daily basis.
My personal journey
During the last 18 years, I’ve been managing this balance decently. The most well-understood metric for diabetes management is A1C. Simply explained, it’s the average blood sugar level over a three month period. My A1C has hovered around 7% for many years, and I’ve been struggling to understand what changes I need to make to improve it. 7% is not bad, but it’s not good either, and it might lead to complications down the line.
A1C levels and their corresponding blood glucose level: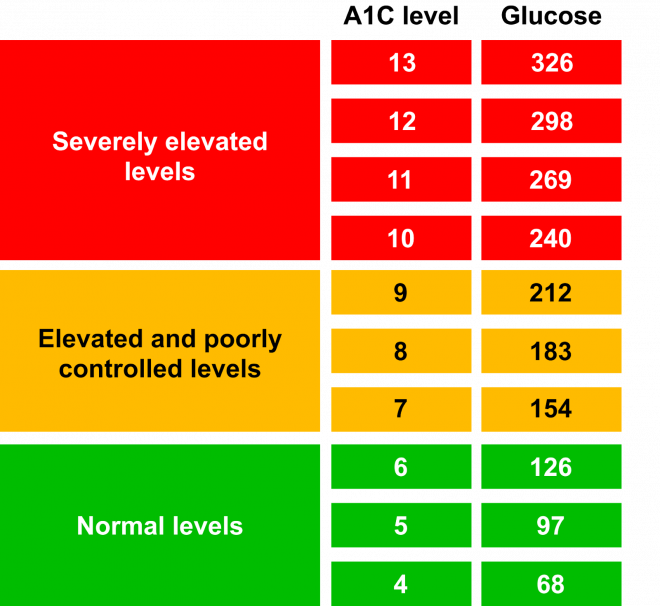
A few months ago that all changed. Over the last couple of years, more than a few people with diabetes had been telling me to get a continuous glucose monitor (CGM) and last year I finally decided to try one out. A CGM is a sensor that you place on your body that continuously measures your blood sugar throughout your day giving you many data points on how your blood glucose levels are changing. The sensor is not connected directly to the bloodstream, but instead measures interstitial fluid and then uses an algorithm to predict the blood sugar level. Having a sensor continuously measuring your blood sugar levels without you having to think about it has several advantages:
- No more pricking your finger several times a day with bulky equipment
- Measure when it was previously impossible, like when working out or sleeping
- More frequent data making it easier to connect highs and lows to specific actions like a meal or work out
12 hour CGM curve from my Nightscout app: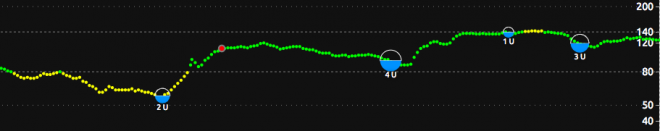
Enabling experimentation
As a product manager, I’ve always believed in the old cliché “You cant improve what you can’t measure” and CGM entering my life has been a testament to that. After trying it out for about a week, I started realizing that I now had a real feedback loop in front of me. A feedback loop that would, almost in real time, tell me how food, physical activity, medication, sleep and other daily inputs affect my blood sugar. So I started doing what product managers always do when they have a feedback loop set up and know what success looks like: run experiments.
To run these experiments I mostly used Excel. I entered my starting blood sugar value, what I was eating and how much insulin I was taking. After two hours I entered what my resulting value was. Using this method, I could not only see what was impacting my blood sugar levels but also how well I was assessing the amount of insulin needed to cover a meal. I kept going, uncovering more insights. For example, playing basketball raises my blood sugar quite a bit, likely due to cortisol released into my body from stress. Since I play every week, I started developing strategies for mitigating some of its effects. When I play nowadays, my blood sugar still rises but not even close to where I used to end up. To be honest, I would likely not even have found out basketball was the reason for my elevated blood sugar levels, because I never would have tested blood sugar during a game!
Screenshot from my Excel sheet filled with experiments: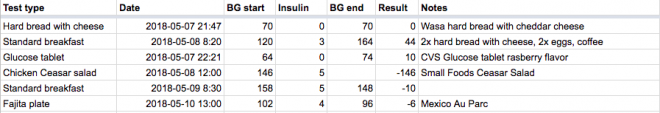
The results
After about four months of testing, iterating, analyzing and making changes, I went to get my first A1C. I had seen pretty dramatic improvements in the data produced by my CGM, but honestly it seemed too good to be true. At the same time I had seen my insulin needs reduced by more than 50% which in itself is a pretty remarkable change. And as a result of my improved diet and lowered insulin dose I had lost 7 lbs, which is something I had been trying to do for a while. Then I got the results: 5.8%. Wow. I was feeling better than ever, on less insulin, had more stable energy levels and had a fantastic A1C. I had no idea this was even possible. Now, some people would ask, does this improvement also mean that you have more lows? It’s hard to tell as there isn’t an as clear metric for hypoglycemia, but anecdotally my feeling is that I’m actually having fewer lows now compared to before.
Why did it take this long?
After processing the changes I had made and the impact it had on my life I started to wonder, why hadn’t I done this earlier? I came to the conclusion that before I had ever tried out a CGM, I wouldn’t have known it would unlock this much value. The behavior it enabled was learning. Learning about how food, physical activity and medication were affecting my blood sugar levels, in an almost real-time way and making it possible to run many experiments in a short amount of time. It also taught me that some of the advice my care provider had given me was not right for me. It turns out that many parameters are different between each person with diabetes. Things like body mass index, metabolism and climate all affect how your body reacts, and even the same kind of food can impact the blood sugar of two persons with diabetes differently. These parameters are today mostly ignored when people with diabetes get advice on how to manage their condition. Even though we now have the data to understand each person on an individual level.
I suspect that one of the reasons that more people haven’t seen the type of results that I have is that getting there took a lot of time. I was fortunate enough to have most of last year off from work so had the opportunity to spend time on my health, whereas most people don’t. And even though I’m an engineer and product person, getting to the insights that were buried deep down in the data from my CGM was not easy. I had to do lots of manual reporting in Excel and repeat tests several times due to high variance and unexpected effects from previous decisions. It also required some knowledge of data analysis and basic script writing. Simply put, I don’t expect many people, even though they get a CGM, to be able to achieve the results I did, which is unfortunate as it has had a tremendous impact on my life.
Introducing Steady Health
It’s now been about 18 months since starting on my journey with CGM and improving my management using data analysis, and I have some exciting updates to share. After seeing the impact it had on my management and my life, I decided to try and understand how many other patients were struggling with similar issues and started interviewing patients all over the country. Through those conversations I realized that diabetes care needs an upgrade.
Over the last few months, I’ve assembled a team to build a new, diabetes focused, care provider that uses data analysis to personalize care for the individual. We’re calling it Steady Health. At Steady our team of doctors, nurses and member guides provide care that is both more impactful and more convenient. We achieve this through a combination of technology enabled remote care and a physical clinic in downtown San Francisco.
If you’re curious and want to find out more, please visit our website or email me directly at henrik@steady.health.





